Signs & Symptoms
of WNV infection
The incubation period before symptoms appear is from 2 to 14 days (most commonly 2-6 days) after becoming infected. The majority of people may not even be aware they are infected. An estimated 70-80% of human WNV infections are subclinical or asymptomatic.
Most symptomatic persons experience an acute systemic febrile illness that often includes headache, weakness, myalgia, or arthralgia; gastrointestinal symptoms and a transient maculopapular rash also are commonly reported. Less than 1% of infected persons develop neuroinvasive disease, which typically manifests as meningitis, encephalitis, or acute flaccid paralysis.
WNV is classified according to presence and severity of symptoms.
- Viremia only
- Mild (West Nile Fever)
- Severe (WNV neurological disorders)
Viremia
Viremia is simply the presence of virus in the blood. About 80% of people who are WNV infected have no obvious signs of infection. They do not feel ill or have any symptoms of infection. It is believed that these people have viremia lasting, on average, 6.5 days. Most people will not be aware they are infected but may be identified through screening, such as when they donate blood.
Instant feedback:
The incubation period for WNV infection is from 2-14 days.
Mild symptoms (West Nile fever)
About 20% of people infected with WNV have mild symptoms. Mild symptoms may persist for days or weeks, but most commonly last 3 to 6 days. This condition is referred to as West Nile fever. An uncomplicated infection is usually characterized by fever of sudden onset (>102.2 F/39 C), often with nausea and vomiting.
West Nile Fever symptoms include the following:
- fever
- headache
- body aches
- nausea & vomiting
- conjunctivitis
- pharyngitis
- swollen lymph glands
- Maculopapular rash on the chest, stomach, and back
Gorsche and Tilley (2005), in the Canadian Medical Association Journal, show a picture of the typical rash associated with WNV:
https://www.cmaj.ca/cgi/content/full/172/11/1440/F122
The rash that is associated with WNV usually appears 3-7 days after the onset of symptoms, along with the onset of fever. The rash usually persists for 7 to 14 days. The rash may begin on the back of the arms and trunk and then spread across the torso, face, and limbs, usually sparing the palms and soles. Typically the rash, as described by Gorsche and Tilley, is erythematous, diffuse, and painful, but doesn’t itch.
The rash consists of discrete, irregularly-shaped macules and slightly elevated papules 2-6 mm in diameter. The rash blanches with finger pressure and some papules are tender to the touch. The frequency of rash associated with WNV has varied somewhat. In New York and New Jersey in 2000, 16% of patients (3 of 19) had a maculopapular rash, and in an outbreak in Ontario in 2002, 27% of patients (17 out of 67) had a similar rash. WNV should be suspected in any patient presenting with a similar rash.
To determine the clinical course of West Nile Fever, the Illinois Department of Health conducted a study which excluded patients exhibiting severe nervous system involvement. Ninety eight (98) patients with West Nile Fever were followed through the course of their disease. The findings suggest that West Nile fever is a more serious illness than previously thought and that there are debilitating effects that persist after the acute phase of the illness:
| Percent |
Symptom |
Median duration/days |
96% |
Fatigue |
36 |
81% |
Fever |
5 |
71% |
Headache |
10 |
61% |
Muscle weakness |
28 |
53% |
Difficulty concentrating |
14 |
About 31% required hospitalization for an average of 5 days. At 30 days after onset of the illness, 63% of respondents continued to have symptoms. Among the 72 patients who normally attended work or school, 57 (79%) could not attend because of illness, and had a median absence of 10 days. The results of this study suggest that there should be more follow-up for patients with West Nile fever after the acute phase of the disease.
Instant feedback:
Most people experience no symptoms after the acute phase of West Nile fever.
Severe neurological symptoms
Approximately 1 in 150 people (less than 1%) infected with WNV will develop severe neurological symptoms, such as WNV-associated meningitis, encephalitis and/or acute flaccid paralysis.
Some neurological patterns have emerged in patients with WNV :
Factor |
Meningitis |
Encephalitis |
Acute Flaccid paralysis |
Age group |
Younger - median 36 yrs |
Elderly - median 70 yrs |
Middle-aged - median 56 yrs |
Presentation |
Acute phase |
After acute phase |
During acute phase |
Mental status |
Normal |
Altered |
Normal or depressed |
Findings |
|
- Fever >38ºC
- CSF pleocytosis
- Personality and LOC changes
- Respiratory depression
- seizure (rare)
- Coma (rare)
|
- Acute asymetric weakness
- Hyporeflexia/areflexia of affected limb
- No loss of sensation
- CSF pleocytosis
- Abnormal MRI signal in anterior horn
- Respiratory arrest (rare)
|
Instant feedback:
Less than 1% of people infected with WNV develop severe neurological symptoms.
WNV-associated meningitis
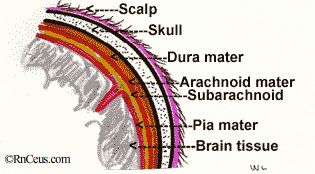 WNV meningitis is a typical aseptic viral meningitis with low mortality. Meningitis is an inflammation of the pia mater and arachnoid membranes which envelop the brain and the spinal cord. It accounts for 20% to 30% of the central nervous system symptoms associated with the virus. The most common symptom is severe headache and fever with back pain, myalgias, and rash in 20% to 50%. Neck stiffness and photophobia occur in 19% to 27%. People should be hospitalized to rule out other causes, which might be more readily treated. Some meningitis progresses to encephalitis.
WNV meningitis is a typical aseptic viral meningitis with low mortality. Meningitis is an inflammation of the pia mater and arachnoid membranes which envelop the brain and the spinal cord. It accounts for 20% to 30% of the central nervous system symptoms associated with the virus. The most common symptom is severe headache and fever with back pain, myalgias, and rash in 20% to 50%. Neck stiffness and photophobia occur in 19% to 27%. People should be hospitalized to rule out other causes, which might be more readily treated. Some meningitis progresses to encephalitis.
Instant feedback:
WNV-associated meningitis is a typical aseptic viral meningitis.
WNV-associated encephalitis
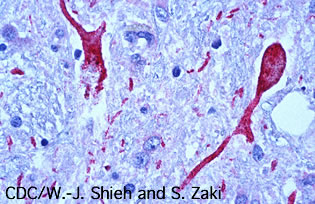
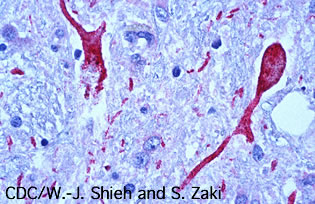
|
Photomicrograph of brain tissue from a West Nile encephalitis patient, showing antigen-positive neurons and neuronal processes (in red). |
Two-thirds of WNV cases with serious neurological involvement manifest as encephalitis or meningoencephalitis. Encephalitis is an inflammation of the brain tissue. It presents multiple symptoms suggesting central nervous system impairment, including headache, fever, weakness, nausea and vomiting. Seizures are uncommon. About 15% of WNV encephalitis cases will progress to coma. Muscle weakness is a prominent symptom and may involve AFP progressing to respiratory failure.
Symptoms have varied in different outbreaks. In Louisiana, in 2002, patients with WNV encephalitis presented with movement disorders, including tremors (often accentuated with movement), myoclonus, and parkinsonian features of cogwheel rigidity, hypokinesia, and postural instability. Several patients had hyperreflexia and bulbar findings, including cranial nerve abnormalities, dysphagia, and altered oculocephalic reflexes. Overall mortaility rate for those with WNV encephalitis range from 4% to 14%; however, death rates are higher for elderly patients.
Instant feedback:
WNV-associated encephalitis can result in coma and death.
WNV-associated acute flaccid paralysis
Acute flaccid paralysis (AFP), is characterized by the acute onset of muscle weakness in limbs and/or respiratory muscles. Severe symptoms may last several weeks and can result in permanent neurological deficits or death.
AFP characterisitics are similar to the poliomyelitis syndrome caused by polio virus. Poliomyelitis involves inflammation of gray matter in the spinal cord, often resulting in paralysis and respiratory failure. WNV related muscle weakness and paralysis are thought to be caused by viral destruction of cells in the anterior horn of the spinal cord.
Other nerves are at risk. WNV is thought to be involved in the demyelination of peripheral nerves resulting in an illness similar to Guillain-Barre syndrome. Cranial nerves can be affected resulting in facial palsey, dysphagia and optic neuritis.
A Colorado study of 219 patients with neuro-invasive disease found that 32 (15%) of those with WNV neuro-invasive disease developed AFP, a rate of 4.4/100,000 population, comparable to poliomyelitis during polio virus epidemics:
| Number |
Percent |
Description |
6 |
19% |
AFP alone (3 with no fever, headache) |
10 |
31% |
AFP and meningitis |
16 |
50% |
AFP and encephalitis |
Among the 32 patients with AFP, there were 3 distinct clinical/ pathological presentations:
- 27 (84%) had asymmetric weakness without sensory loss,
- 12 weakness in all limbs,
- 11 facial nerve palsy,
- 11 acute respiratory failure requiring intubation
- 5 neuronmuscular respiratory weakness, not requiring intubation.
- 4 (13%) had symmetric ascending weakness with sensory abnormalities consistent with an acute inflammatory demyelinating polyradiculoneuropathy form of Guillain-Barré syndrome,
- 1 with acute respiratory failure requiring intubation.
- 1 (3%) had shoulder abduction weakness consistent with a long thoracic nerve paralysis
At a 3-month followup, 2 could not be found, 3 had died, so only 27 could be evaluated. The followup showed the following:
- AFP
- 7 minimal or no improvement
- 15 some improvement in strength with 12 using ambulatory aids, orthotics
- Guillain Barre
- 3 of 4 patients had good outcome
- Shoulder weakness
- 1 patient had no improvement, but little functional difficulty
Of the 12 patients with acute respiratory weakness, 3 died, 2 were still on chronic ventilation, and the median duration of intubation was 66 days. Early dysarthria and dysphagia were consistent with impending respiratory failure.
It’s important for healthcare providers to recognize that symptoms of AFP can occur without meningitis or encephalitis or even headache or fever. There may be few clues other than weakness to suggest the patient is suffering from severe WNV infection. Researchers do not yet know the long term effects on patients.
Instant feedback:
WNV-associated AFP syndrome is similar to that caused by the polio virus.
© RnCeus.com
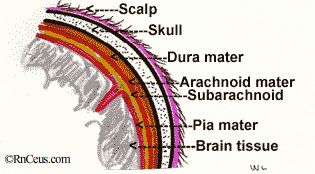 WNV meningitis is a typical aseptic viral meningitis with low mortality. Meningitis is an inflammation of the pia mater and arachnoid membranes which envelop the brain and the spinal cord. It accounts for 20% to 30% of the central nervous system symptoms associated with the virus. The most common symptom is severe headache and fever with back pain, myalgias, and rash in 20% to 50%. Neck stiffness and photophobia occur in 19% to 27%. People should be hospitalized to rule out other causes, which might be more readily treated. Some meningitis progresses to encephalitis.
WNV meningitis is a typical aseptic viral meningitis with low mortality. Meningitis is an inflammation of the pia mater and arachnoid membranes which envelop the brain and the spinal cord. It accounts for 20% to 30% of the central nervous system symptoms associated with the virus. The most common symptom is severe headache and fever with back pain, myalgias, and rash in 20% to 50%. Neck stiffness and photophobia occur in 19% to 27%. People should be hospitalized to rule out other causes, which might be more readily treated. Some meningitis progresses to encephalitis.