Ventricular Septal Defects and the Eisenmenger Effect
 Eisenmenger syndrome (ES) is an advanced form of pulmonary arterial hypertension (PAH) associated with congenital heart defects (CHD). Several types of CHD can increase both pulmonary blood flow and pressure, eventually causing progressive damage to the pulmonary vasculature. The cardiac defects most commonly associated with ES include ventricular septal defects (VSDs), atrial septal defects (ASDs), atrioventricular septal defects, and patent ductus arteriosus. Early surgical correction of these defects has significantly reduced the incidence of ES. However, once PAH has developed, surgical correction is contraindicated.
Eisenmenger syndrome (ES) is an advanced form of pulmonary arterial hypertension (PAH) associated with congenital heart defects (CHD). Several types of CHD can increase both pulmonary blood flow and pressure, eventually causing progressive damage to the pulmonary vasculature. The cardiac defects most commonly associated with ES include ventricular septal defects (VSDs), atrial septal defects (ASDs), atrioventricular septal defects, and patent ductus arteriosus. Early surgical correction of these defects has significantly reduced the incidence of ES. However, once PAH has developed, surgical correction is contraindicated.
Pathophysiology of Eisenmenger Syndrome
The 2022 JACC State-of-the-Art Review provides an in-depth analysis of the pathophysiology of ES, emphasizing the following key points:
-
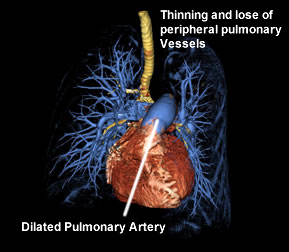 |
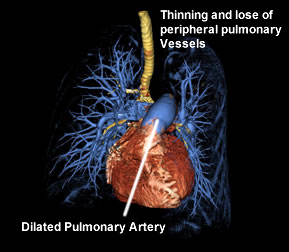
| Computed tomography 3D surface rendering of the lungs and heart from a patient with pulmonary arterial hypertension demonstrating trachea and major airways (yellow), an enlarged heart (red), enlarged main pulmonary artery (large blue vessel on top of heart) and thinning of the peripheral pulmonary vessels (blue). Marcus Y. Chen, M.D., (NHLBI 2022) |
Uncorrected Left-to-Right Shunt: An uncorrected left-to-right shunt increases pulmonary artery pressure and blood flow.
- Shear Stress and Endothelial Injury: Increased blood flow causes shear stress on the endothelium and circumferential stretch of the pulmonary artery
walls.
-
Vascular Remodeling: Endothelial stress leads to vascular remodeling, characterized by inflammation, intimal proliferation of smooth muscle, extracellular matrix deposition, and intravascular thrombosis.
- Increased Pulmonary Vascular Resistance (PVR): Smooth muscle proliferation thickens the pulmonary arteriole walls and narrows the lumen, while extracellular matrix deposition decreases compliance. The combination of narrowed lumen and stiffened vessel walls increases PVR.
- Right Heart Strain and Shunt Reversal: Elevated PVR raises right heart pressures, resulting in right ventricular hypertrophy and ultimately reversing the shunt.
- Hypoxemia and Cyanosis: The now right-to-left shunt reduces systemic arterial oxygen saturation, a defining characteristic of Eisenmenger syndrome (Arvanitaki 2022).
Symptoms of ES differ with the type of CHD and with age. Patients with uncorrected atrial septal defects (ASD) may not develop symptoms until 20 to 40 years of age (Beerman 2020). While patients with VSD, patent ductus arteriosus, or more complex defects may develop symptoms in infancy or early childhood, depending on the size of the defect and the rate of pulmonary vascular remodeling (Frank, 2015).
Common signs and symptoms include:
- Pulmonary hypertension – elevated pressure in the precapillary vessels of the lungs
- Shortness of breath (exertional dyspnea)
- Fatigue
- Lethargy
- Exercise intolerance
- Syncope
- Cyanosis
- Right heart failure
- Orthopnea
- Paroxysmal nocturnal dyspnea
- Peripheral edema
- Ascites
- Hepatomegaly
- Jugular venous distention
ES epidemiology
Eisenmenger syndrome (ES) is a severe form of pulmonary arterial hypertension (PAH) associated with congenital heart defects (CHD). The prevalence of ES varies: it is encountered in approximately 1% to 5.6% of large tertiary CHD cohorts. Among patients with PAH associated with CHD, the prevalence of ES ranges from 1.1% to 12.3%, depending on the registry and population studied. The incidence of ES has declined in high-income countries due to early diagnosis and surgical correction of CHD. However, in low- and middle-income countries, ES remains more prevalent due to limited access to timely medical care and surgical interventions (Arvanitaki 2022).
Treatment
- Curative treatment for Eisenmenger Syndrome requires heart-lung transplant.
- Palliative medical treatment focuses on managing the symptoms and complications
- pulmonary vasodilation
- prostacyclin analogs: treprostinil, epoprostenol
- endothelin antagonist: bosentan
- nitric oxide enhancers sildenafil
- supplemental O2
- Phlebotomy in the event of erythrocytosis with hyperviscosity in response to chronic hypoxia (Oechslin 2010)
- Antithrobotic drugs
- Endocarditis prophylaxis before dental or surgical procedures that are likely to cause bacteremia.(Beerman 2020)
Instant Feedback:
What
direction is the shunt in an Eisenmenger effect:
References
Arvanitaki, A., Gatzoulis, M. A., Opotowsky, A. R., Khairy, P., Dimopoulos, K., Diller, G.-P., Giannakoulas, G., Brida, M., Griselli, M., Grünig, E., Montanaro, C., Alexander, P. D., Ameduri, R., Mulder, B. J. M., & D’Alto, M. (2022). Eisenmenger syndrome: JACC state-of-the-art review. Journal of the American College of Cardiology, 79(12), 1183–1198. https://doi.org/10.1016/j.jacc.2022.01.022
Beerman, L. B. (2022, April 18). Eisenmenger syndrome - Pediatrics. Merck Manuals Professional Edition. Retrieved May 1, 2022, from https://www.merckmanuals.com/professional/pediatrics/congenital-cardiovascular-anomalies/eisenmenger-syndrome
Frank, D. B., & Hanna, B. D. (2015). Pulmonary arterial hypertension associated with congenital heart disease and Eisenmenger syndrome: current practice in pediatrics. Minerva pediatrica, 67(2), 169–185.
Oechslin, E., Mebus, S., Schulze-Neick, I., Niwa, K., Trindade, P. T., Eicken, A., Hager, A., Lang, I., Hess, J., & Kaemmerer, H. (2010). The Adult Patient with Eisenmenger Syndrome: A Medical Update after Dana Point Part III: Specific Management and Surgical Aspects. Current cardiology reviews, 6(4), 363–372. https://doi.org/10.2174/157340310793566127
 Eisenmenger syndrome (ES) is an advanced form of pulmonary arterial hypertension (PAH) associated with congenital heart defects (CHD). Several types of CHD can increase both pulmonary blood flow and pressure, eventually causing progressive damage to the pulmonary vasculature. The cardiac defects most commonly associated with ES include ventricular septal defects (VSDs), atrial septal defects (ASDs), atrioventricular septal defects, and patent ductus arteriosus. Early surgical correction of these defects has significantly reduced the incidence of ES. However, once PAH has developed, surgical correction is contraindicated.
Eisenmenger syndrome (ES) is an advanced form of pulmonary arterial hypertension (PAH) associated with congenital heart defects (CHD). Several types of CHD can increase both pulmonary blood flow and pressure, eventually causing progressive damage to the pulmonary vasculature. The cardiac defects most commonly associated with ES include ventricular septal defects (VSDs), atrial septal defects (ASDs), atrioventricular septal defects, and patent ductus arteriosus. Early surgical correction of these defects has significantly reduced the incidence of ES. However, once PAH has developed, surgical correction is contraindicated.