The lower urinary tract (LUT) is comprised of the urinary bladder, the urethra and the prostate in men. The function of the LUT is the storage of urine and its voluntary expulsion from the body. These mutually exclusive states are mediated by complex neural networks (Sekhon & Ballaro, 2022). This neural system coordinates the activity of the urinary bladder and an outlet including bladder neck, urethra, and striated muscles of the pelvic floor. During the storage phase, the outlet is closed and the bladder is quiescent to maintain a low intravesical pressure and continence, and during the voiding phase, the outlet relaxes and the bladder contracts to promote efficient release of urine (Wada, N. 2022).
Urinary Bladder
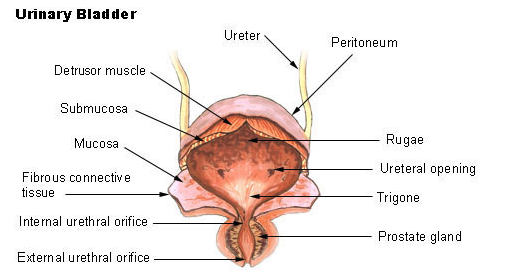
The urinary bladder is a temporary storage reservoir for urine. It is located posterior to the symphysis pubis, and below the parietal peritoneum. The size and shape of the urinary bladder varies with the amount of urine it contains and with the pressure it receives from surrounding organs.
The inner lining of the urinary bladder is a mucous membrane of transitional epithelium that is continuous with that in the ureters. When the bladder is empty, the mucosa has numerous folds called rugae. The rugae and transitional epithelium allow the bladder to expand as it fills.
The second layer in the walls is the submucosa, which supports the mucous membrane. It is composed of connective tissue with elastic fibers.
The next layer is the muscularis, which is composed of smooth muscle. The smooth muscle fibers are interwoven in all directions and, collectively, these are called the detrusor muscle. Contraction of this muscle expels urine from the bladder. On the superior surface, the outer layer of the bladder wall is parietal peritoneum. In all other regions, the outer layer is fibrous connective tissue.
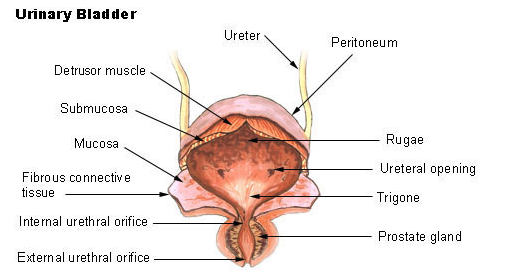
The trigone is between the three openings in the floor of the urinary bladder. Two of the openings are from the ureters and form the base of the trigone. Small flaps of mucosa cover these openings and act as valves that allow urine to enter the bladder but prevent it from backing up from the bladder into the ureters. The third opening, at the apex of the trigone, is the opening into the urethra. A band of the detrusor muscle encircles this opening to form the internal urethral sphincter (Urinary bladder, n.d.).
 Bladder function
Bladder function
The innervation of the detrusor is different from that of the bladder neck.
Micturition by parasympathetic reflex (involuntary emptying)
Involuntary parasympathetic reflex voiding occurs in infants and children until the age of 3-5 years, after which it becomes voluntary (Fowler, 2008). It also can occur after a supra-sacral spinal cord injury that blocks impulses to or from the Pons, resulting in the reflex or involuntary contraction of the bladder.
Parasympathetic innervation originates in the sacrum and serves to promote urination. Parasympathetic nerves activate the detrusor muscle causing it to contract and to relax the internal sphincter (Rahman, 2022).
Urine storage mode sustained by sympathetic dominance (adult voluntary voiding)
Sympathetic innervation originates in the L1,L2 segments of the spinal cord and serves to inhibit urination. Sympathetic nerves inhibit the detrusor muscle and activate the internal sphincter to contract (Rahman, 2018).
References
Fowler, C. J., Griffiths, D., & de Groat, W. C. (2008). The neural control of micturition. Nature reviews. Neuroscience, 9(6), 453–466. https://doi.org/10.1038/nrn2401
Griffin, C.S., Thornbury, K.D., Hollywood, M.A. et al. Muscarinic receptor-induced contractions of the detrusor are impaired in TRPC4 deficient mice. Sci Rep 8, 9264 (2018). https://doi.org/10.1038/s41598-018-27617-5
LeBouef T, Yaker Z, Whited L. Physiology, Autonomic Nervous System. [Updated 2022 May 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538516/
Rahman M, Siddik AB. Neuroanatomy, Pontine Micturition Center. [Updated 2022 Sep 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557419/
Sekhon, N., & Ballaro, A. (2022). The physiology and pharmacology of the lower urinary tract. Surgery (Oxford), 40(8), 501–507. https://doi.org/10.1016/j.mpsur.2022.05.003
Urinary bladder. Urinary Bladder | SEER Training. (n.d.). Retrieved February 26, 2023, from https://training.seer.cancer.gov/anatomy/urinary/components/bladder.html
Wada N;Karnup S;Kadekawa K;Shimizu N;Kwon J;Shimizu T;Gotoh D;Kakizaki H;de Groat WC;Yoshimura N; (n.d.). Current knowledge and novel frontiers in lower urinary tract dysfunction after spinal cord injury: Basic research perspectives. Urological science. Retrieved February 26, 2023, from https://pubmed.ncbi.nlm.nih.gov/36177249/