What to Do While the Patient is
Unconscious
While each patient's unconscious experience is
unique, there are some activities which are almost universally
helpful.
HOW TO HELP
1. Encourage all of the emotionally positive
people in the person's life to visit. Many patients report
feeling the amount of caring these people bring with them. While
most hospitals have policies that allow only the immediate family
in ICUs, this policy is intended to be for the well-being of the
patient. Many hospitals are flexible if a visit from a close
friend or even a pet would be helpful.
2. Similarly, try to discourage or prevent
people from visiting who might drain your patient with their
negativity. Abusive parents and spouses should not be allowed to
visit. At the moment, your patients can only protect themselves
by retreating further into their unconscious state. This is the
opposite effect to what you are trying to achieve. This advice is
particularly important if your patient is suffering from a
distorted perception of the situation. If they already think they
are being held captive, the presence of someone who has brought
them harm in the past exacerbates the situation.
3. Remember that your patients may be able to
sense many of things going on around them. They may be able to
hear, feel, or even see you. Because of this, try to talk to,
not about your patient. If they are unable to communicate
with you, but can still sense what is going on around them, they
are most likely very frightened and frustrated. Even reports of
the seemingly inconsequential occurrences at home may give them
great comfort. It is extremely important to remember this
suggestion, as many patients report hearing most discouraging
comments. Always treat them as if they are completely awake.
4. The above advice is particularly important
to remember when unconsciousness has just occurred, the patient
is coming out of unconsciousness, or has just been moved.
5. Remember that your patient's personality has
not changed. If they did not like sports on television before
they became unconscious, they do not like it now. Try to arrange
the environment in the way your patient might if they were awake.
If they have always enjoyed physical contact, like hugging or
holding hands, have the family keep doing that. Try to be aware
of their likes and dislikes in the past and try to arrange the
environment accordingly.
6. Ask the family to bring in photos of your
patient doing activities that are important to him/her. The
photos can help you and the other staff understand your patient
more as a person.
7. If your patient is struggling against their
tubing, or trying to get out of bed, they may be suffering from
the previously discussed distorted awareness. Remember that this
is very frightening to them. Remain very calm and keep explaining
to your patient where they are, what is happening to them, and
that you are there.
8. Maintain a schedule similar to that of the
patient's normal routine. If he/she is an early riser, let the
staff know and have them promote the same schedule.
9. Watch for signs of awareness. While some
research is being done to detect awareness through sophisticated
equipment, what you observe can be very meaningful. Some early
signs of awareness can be observed in facial expressions, eye
expressions, and appropriate tears.
Instant Feedback:
Encourage
emotionally significant individuals to visit the patient even if
they are not relatives.
 Denney (2008) researched the effects of compassionate presence on people in comatose state measured by the Heart Math Freeze-Framer heart monitoring program. The HeartMath Freeze-Framer heart monitoring program detects heart rate variability which can detect changes in external and internal conditions. The rhythm of a healthy heart is surprisingly irregular even when resting. The beat-to-beat changes in heart rate is called heart rate variability (HRV).
Denney (2008) researched the effects of compassionate presence on people in comatose state measured by the Heart Math Freeze-Framer heart monitoring program. The HeartMath Freeze-Framer heart monitoring program detects heart rate variability which can detect changes in external and internal conditions. The rhythm of a healthy heart is surprisingly irregular even when resting. The beat-to-beat changes in heart rate is called heart rate variability (HRV).
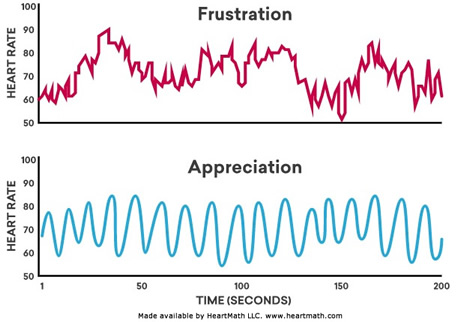
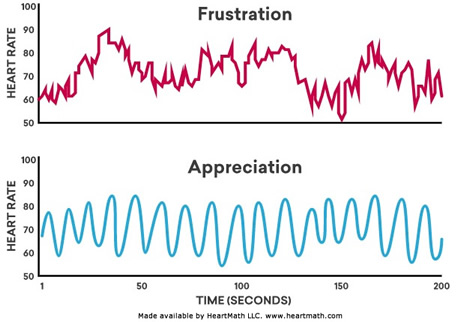
The HeartMath Institute has researched the different patterns of heart activity that correlate with different emotional states. For example, during stress and negative emotions such as including emotions such as anger, frustration, and anxiety the heart rhythm tends to be erratic and disordered.
A more ordered and stable heart pattern, called coherence, indicates a positive emotional state such as appreciation, joy, care, and love (Made available by HeartMath LLC. www.heartmath.com).
In this study, Denney tested for the presence of nonverbal interaction between a patient in a comatose state and a sitter in a compassionate state of presence with that patient. Four hospice patients who were comatose and seven sitters, who were hospice volunteers, participated in the study. The sitters were to be in a state of compassionate presence. They spent 20 to 30 minutes with the patients at each session. FreezeFramer® finger sensors were used for both the patients and sitters.
Comparisons with available baselines showed that patients had an increase in coherence in 14 out of 28 sittings, and a decrease in patient coherence in 6 out of 28 sittings. It appeared from the study the patients were sensitive to people in their environment.
Machado-Ferrer, et al. (2013) assessed heart rate variability of comatose patient with different Glasgow Coma Scale scores. The Glasgow Coma requires subjects to be able to move, which many perceived to be unconscious subjects said they cannot do. That needs to be considered when interpreting this study. The researchers compared HRV between 16 comatose patients and 22 normal subjects. The researchers found the HRV to be reduced in patients, particularly those with GCS = 3. The also concluded the HRV procedure, which is minimally invasive and low cost, is a powerful tool to assess the ANS in comatose patients.
The measurement of HRV in ICUs patients who are unconscious seems a very viable option. Several other researchers have carried out research in ICUs using HRV measurements. To date, no research has included turning or otherwise moving patients with the intent of increasing consciousness and then measuring HRVs.
The studies reported in this course highlight a need in the perceived to be unconscious patients to have human connections and communications. HRV assessments can assist health professionals and friends and family members detect these positive as well as negative connections.
References
Denney, J.M. (2008). The Effects of Compassionate Presence on People in Comatose States Near Death. USABPJ. 7(2). https://www.ibpj.org/issues/archive/Vol7No2%20USABP%20Journal%202008.pdf#page=11.
Machado-Ferrer, Y., Estévez, M., Machado, C., Hernández-Cruz, A., Carrick F.R., Leisman, G. et al. (2013). Heart rate variability for assessing comatose patients with different Glasgow Coma Scale scores. Clin Neurophysiol. 124(3),589-97.
©RnCeus.com
 Denney (2008) researched the effects of compassionate presence on people in comatose state measured by the Heart Math Freeze-Framer heart monitoring program. The HeartMath Freeze-Framer heart monitoring program detects heart rate variability which can detect changes in external and internal conditions. The rhythm of a healthy heart is surprisingly irregular even when resting. The beat-to-beat changes in heart rate is called heart rate variability (HRV).
Denney (2008) researched the effects of compassionate presence on people in comatose state measured by the Heart Math Freeze-Framer heart monitoring program. The HeartMath Freeze-Framer heart monitoring program detects heart rate variability which can detect changes in external and internal conditions. The rhythm of a healthy heart is surprisingly irregular even when resting. The beat-to-beat changes in heart rate is called heart rate variability (HRV).