Liver Decompensation
The liver is critical to survival. When injury from viral infection, chemical toxicity, ischemia or autoimmune inflammation damage or kill liver cells, the remaining cells can compensate by doubling their metabolic function. If liver injury or cell loss outstrips its ability to compensate, the liver functions of biotransformation, glycogenolysis, gluconeogenesis, protein synthesis, filtration, etc., will diminish.
As the liver fails, the body will exhibit signs of hepatic insufficiency. Minor signs including: nausea, diarrhea, anorexia and fatigue. More serious liver decompensation is associated systemic signs and symptoms.
- Central Nervous Systems
- Altered Mental Status
- (Encephalopathy)
- Asterixis
- Cerebral edema
- Hematological
- Thrombocytopenia
- Coagulopathy
- Hyperbilirubinemia >2
- Cardiovascular
- Hypotension
- Portal hypertension
|
- Metabolic
- Hypoglycemia
- Feotor hepaticus
- Hepatorenal syndrome
- Splanchic arterial vasodilatation
- Na+ & H20 retention, ascites
- Endocrine
- Testicular atrophy
- Gynecomastia
- Menstrual irregularities
- Respiratory
- Hepatopulmonary Syndrome
- Pleural effusion
|
- Skin
- Pruritus
- Spider angiomas
- Palmer erythema
- GI
- N/V
- Malnutrition
- Spontaneous bacterial peritonitis
- Immunologic
- Phagocytic dysfunction
- Complement deficiency
- Sepsis
|
- Liver
- Hypoproteinemia
- Cholestasis
- Jaundice
- Pain
- Musculoskeletal
- Dupuytrens contracture
- Osteoarthropathy
- Muscle wasting
|
Acute Liver Failure
ALF Classification |
Causes of ALF in the U.S.* |
- Hyperacute - jaundice to encephalopathy 0-7 days
- Acute - jaundice to encephalopathy 8-28 days
- Subacute - jaundice to encephalopathy 29-84 days
|
- Acetaminophen overdose 46%
- Unknown 14%
- Drug/toxin reactions 12% (antibiotics, NSAIDs, anticonvulsants)
- Hepatitis B virus 7.7%
- Autoimmune Hepatitis 5.9%
- Ischemia 4.6%
- Hepatitis A virus 2.6%
- Wilson disease 1.4%
- Budd-Chiari syndrome 0.9%
- Pregnancy 0.8%
- Other 4.8%
|
Acetaminophen Toxicity
Acetaminophen is oxidized to the toxic metabolite N-acetyl-p-benzoquinone imine (NAPQI).At normal therapeutic dosage any NAPQI produced is rapidly neutralized by the chief hepato-cellular anti-oxidant, glutathione. Neutralizing NAPQI depletes available stores of glutathione. If the amount of NAPQI exceeds available glutathione the hepatocyte is exposed to oxidative damage which can cause inflammation or cell death. Glutathione is also consumed in the process of neutralizing the metabolic by-products of ethanol. Therefore, consuming ethanol with acetaminophen increases the toxicity of acetaminophen or any other source of oxidative stress.* |
(ALF) also known as fulminant hepatic failure is a rare life threatening syndrome that can mimic sepsis.
It is characterized by:
- Abrupt loss of liver function affecting a previously asymptomatic patient,
- Coagulopathy (INR >1.5),
- Decreases sytemic vascular resistance (SVR) Tachycardia and circulatory insufficiency
- Encephalopathy. Cerebral edema is common
- Acute liver failure has been classified as "hyperacute", "acute" and "subacute" based upon the time from jaundice to hepatic encephalopathy (HE).*
The etiology of ALF varies demographically.
- In developing countries, viral hepatitis predominates. Usually HBV, but many others including hemorrhagic fevers
- In developed countries, toxins are the most common cause.
- In the U.S., hyperacute liver failure is usually caused by acetaminophen overdose.
Acetaminophen overdose with a jaundice to encephalopathy interval of 0-7 days has a fair likelihood of spontaneous recovery. A jaundice-to-encephalopathy interval of >28 days is usually caused by idiosyncratic drug reactions. It has a very poor prognosis without liver transplantation. Improvements in intensive care and liver transplantation have significantly affected survival rates. Today a U.S. patient receiving care in a liver transplant center has about a 40% chance of spontaneous recovery and about 65% survival rate following liver transplantation.*
Pathology of ALF:
- Neurologic
- Hepatic encephalopathy (HE) can be divided into four stages: 1) mood/behavioral changes, 2) lethargy and confusion, 3) stupor, 4) coma
- Asterixis: the inability to maintain posture due to a metabolic encephalopathy. On physical exam have the patient extend their arms and bend their hands back resulting in a “flapping” motion consistent with asterixis.
- Cerebral vascular dilitation possibly due to increased systemic nitric oxide
- Cerebral edema: liver failure decreases hepatic conversion of ammonia, produced by intestinal flora, to urea for excretion. Hyperammonemia exposes astrocytes in the brain. Astrocytes convert ammonia to osmotically active nontoxic glutamine. Excess glutamine causes astrocyte swelling and brain edema, which increase ICP.
- Cardiovascular
- Hypotension mimicking sepsis
- Low SVR
- Elevated HR and cardiac output
- Hematologic
- Hyperbilirubinemia/jaundice
- Decreased coagulation factor synthesis.
- Thrombocytopenia
- Vitamin K deficiency
- GI
- Gastrointestinal bleeding
is rare
- Malnutrition
- Endocrine
- Hypoglycemia
- Metabolic acidosis
- Adrenal insufficiency
- Immune system
- Up to 80% of ALF patients
experience life threatening infections due to:
- Invasive ICU instrumentation and catheter related infection.
- Dysfunction of monocytes, neutrophils, kupffer cells, and complement system.
Diagnosis
- Chronology of symptoms including the presentations of jaundice and hepatic encephalopathy.
- Preexisting disease, medications, herbs, dietary supplements, recreational drugs, possible toxic exposures, international travel and lifestyle risks.
- Labs to determine etiology and rule out the presence of chronic liver disease or sepsis.
Treatment:
- Stabilize the patient, transfer to ICU
- Coma care
- Fluid management
- Metabolic management
- Diagnosis of ALF dictates transport to a liver transplant center and placement on the liver transplant list appropriate. Management of multi-organ system failure (MOSF) often complicates ALF and is best managed in an experienced facility capable of providing transplant if indicated. Patients with an INR >2 or a Grade 2 hepatic encephalopathy or whose prognosis is poor due to age and etiology should be considered for transfer to a liver transplant center where experienced professionals can evaluate for transplant listing.*
- If acetaminophen overdose is suspected, IV administration of N-acetylcysteine is the first line of treatment. N-acetylcysteine assists remaining hepatocytes to replace glutathione needed to reduce further oxidative stress.
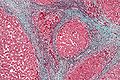 Chronic Liver Disease (CLD) and cirrhosis combined were the 12th most frequent cause of death in the U.S. in 2004.* CLD by definition is a liver illness which has not resolved within 6 months. CLD is characterized by progressive replacement of hepatocytes by fibrosis and eventual cirrhosis. The scar tissue associated with fibrosis and cirrhosis disrupts liver architecture obstructing blood flow and bile excretion. Cirrhotic scarring eventually isolates and encapsulates islands of hepatocytes. Cirrhosis is the common end stage for most chronic liver diseases.
Chronic Liver Disease (CLD) and cirrhosis combined were the 12th most frequent cause of death in the U.S. in 2004.* CLD by definition is a liver illness which has not resolved within 6 months. CLD is characterized by progressive replacement of hepatocytes by fibrosis and eventual cirrhosis. The scar tissue associated with fibrosis and cirrhosis disrupts liver architecture obstructing blood flow and bile excretion. Cirrhotic scarring eventually isolates and encapsulates islands of hepatocytes. Cirrhosis is the common end stage for most chronic liver diseases.
Symptoms of cirrhosis reflect a loss of hepatocyte function resulting in symptoms which include:
- Malnutrition
- Cholestasis
- Jaundice
- Pruritus
- Portal hypertension
- Coagulapathy
- Ascites and edema
- Kidney failure
- Esophageal varices
- Hepatic encephalopathy
- telangiectasia
- Splenomegaly
- Peripheral neuropathy
- Gynecomastia
Diagnosis of cirrhosis is made based upon:
- History of alcohol, viral or drug induced hepatitis
- Physical findings of firm, enlarged liver and symptoms associated with cirrhosis.
- Abnormal laboratory values - prothrombin time, serum proteins, aminotransferases - aspartate (AST) and alanine (ALT), alkaline phosphatase and bilirubin.
- Iimaging studies are useful in identifying and qualifying complications of cirrhosis
- Biopsy is the gold standard to confirm and stage cirrhosis.
Cirrhosis is classified by morphology:
- Micronodular - small nodules <3mm, with thick regular septa, uniformly distributed
- Macronodular - Septa and nodules of varying size. Larger nodules may contain portal tracts.
- Mixed - a combination of micronodular and macronodular
Treatment of cirrhosis is focused on slowing progression and the risk of complications associated with the underlying cause:
- Alcohol abstinence is a prominent component of every cirrhosis management plan
- Chronic hepatitis B and C are treated with pegylated interferon plus an appropriate antiviral
- Autoimmune hepatitis is treated with the corticosteroid prednisone and also sometimes immunosuppressants
- Cholestasis may be treated with ursodeoxycholic acid to protect against cytotoxic bile acids, stimulate bile salt transport, modify immune response
- Nonalcoholic Fatty Liver Disease (NAFLD) and Nonalcoholic Steatohepatitis (NASH) are usually managed with diet and exercise
- Hemochromatosis is treated with phlebotomy
- Wilson disease is treated by chelation with D-penicillamine, trientine or zinc therapy
©RnCeus.com
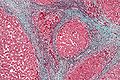 Chronic Liver Disease (CLD) and cirrhosis combined were the 12th most frequent cause of death in the U.S. in 2004.* CLD by definition is a liver illness which has not resolved within 6 months. CLD is characterized by progressive replacement of hepatocytes by fibrosis and eventual cirrhosis. The scar tissue associated with fibrosis and cirrhosis disrupts liver architecture obstructing blood flow and bile excretion. Cirrhotic scarring eventually isolates and encapsulates islands of hepatocytes. Cirrhosis is the common end stage for most chronic liver diseases.
Chronic Liver Disease (CLD) and cirrhosis combined were the 12th most frequent cause of death in the U.S. in 2004.* CLD by definition is a liver illness which has not resolved within 6 months. CLD is characterized by progressive replacement of hepatocytes by fibrosis and eventual cirrhosis. The scar tissue associated with fibrosis and cirrhosis disrupts liver architecture obstructing blood flow and bile excretion. Cirrhotic scarring eventually isolates and encapsulates islands of hepatocytes. Cirrhosis is the common end stage for most chronic liver diseases.