Signs of Inhalant Use and Intoxication
The American Psychiatric Association (2013) classifies significant inhalant abuse as a psychiatric disorder. The following is the American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). https://doi.org/10.1176/appi.books.9780890425596 definition for inhalant abuse:
DSM-5 defines inhalant use disorder as a "problematic pattern of use of a hydrocarbon-based inhalant substance leading to clinically significant impairment or distress.”
Signs of inhalant abuse can include:
- Chemical odors on breath or clothing
- Paint or other stains on face, hands, or clothes
- Hidden empty spray paint or solvent containers, and chemical-soaked rags or clothing
- Drunk or disoriented appearance
- Slurred speech
- Nausea or loss of appetite
- Inattentiveness, lack of coordination, irritability, and depression (NIDA, 2020)
Instant Feedback:
A sign of inhalant use can be as general as nausea, or as specific as chemical odor on clothing.
Inhalant Intoxication
Inhalant intoxication occurs within minutes and generally subsides in approximately 1 hour. The inhalant abuser that has recently been inhaling typically presents with a disheveled appearance, chemical odor on the breath and clothes, and stains on skin and clothes.
Inhalants have high lipid solubility and volatility. That inables the following to occur:
- Rapid absorbtion across pulmonary membranes into the bloodstream
- Crossing the blood-brain barrier
- 15 to 45 minutes of euphoria
- Eventual CNS depression
The CNS depression can lead to lethargy, somnolence, headache, ataxia, stupor, and possible seizures (Tormoehlen et al., 2014). Extreme intoxication may result in sleeplessness, general muscle weakness, dysarthria, nystagmus, and, occasionally, hallucinations or disruptive behavior.
The National Institute on Drug Abuse (NIDA 2020) cites an array of severe consequences of inhalant abuse, including:
 Death from asphyxia, mechanical suffication and fatal accidents
Death from asphyxia, mechanical suffication and fatal accidents- Central and peripheral demyelinating neurotoxicity
- Substance specific hazards
- amyl nitrite, butyl nitrite ("poppers," "video head cleaner")
sudden sniffing death syndrome, suppressed immunologic function (infections and tumors), injury to red blood cells (interfering with oxygen supply to vital tissues)
- benzene (found in gasoline)
bone marrow injury, impaired immunologic function, increased risk of leukemia, reproductive system toxicity
- butane, propane (found in lighter fluid, hair and paint sprays)
sudden sniffing death syndrome via cardiac effects, serious burn injuries (because of flammability)
- freon (used as a refrigerant and aerosol propellant)
sudden sniffing death syndrome, respiratory obstruction and death (from sudden cooling/cold injury to airways), liver damage
- methylene chloride (found in paint thinners and removers, degreasers)
reduction of oxygen-carrying capacity of blood, changes to the heart muscle and heartbeat
- nitrous oxide ("laughing gas"), hexane
death from lack of oxygen to the brain, altered perception and motor coordination, loss of sensation, limb spasms, blackouts caused by blood pressure changes, depression of heart muscle functioning
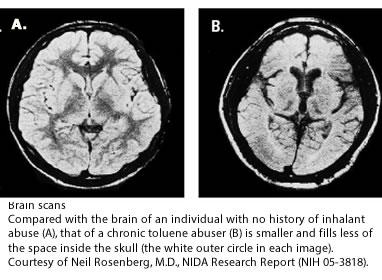
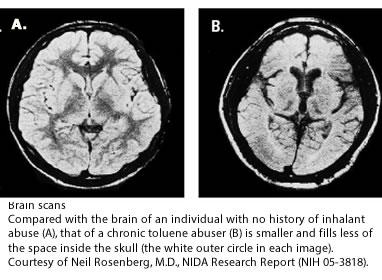
- toluene (found in gasoline, paint thinners and removers, correction fluid)
brain damage (loss of brain tissue mass, impaired cognition, gait disturbance, loss of coordination, loss of equilibrium, limb spasms, hearing and vision loss), liver and kidney damage
- trichloroethylene (found in spot removers, degreasers)
sudden sniffing death syndrome, cirrhosis of the liver, reproductive complications, hearing and vision damage
Instant Feedback:
Inhalants enter the bloodstream quickly and are readily transported to the brain.
References
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). https://doi.org/10.1176/appi.books.9780890425596
NIDA. 2020, May 20. What are the other medical consequences of inhalant abuse?. Retrieved from https://www.drugabuse.gov/publications/research-reports/inhalants/what-are-other-medical-consequences-inhalant-abuse on 2021, September 9
Tormoehlen, L.M., Tekulve, K.J. & Nanagas, K.A. (2014). Hydrocarbon toxicity: a review. Clin Toxicol 52(5), 479–489.
© RnCeus.com
 Death from asphyxia, mechanical suffication and fatal accidents
Death from asphyxia, mechanical suffication and fatal accidents