 The National Quality Forum (2006) definition of hospice care
The National Quality Forum (2006) definition of hospice careHospice Today
 The National Quality Forum (2006) definition of hospice care
The National Quality Forum (2006) definition of hospice care
Hospice is a patient service delivery system that provides palliative care for patients who have a limited life expectancy and require comprehensive biomedical, psychosocial, and spiritual support as they enter the terminal stage of an illness or condition. It also supports family members coping with the complex consequences of illness, disability, and aging as death nears (p.3). In 2014, approximately 1.6 to 1.7 million people received hospice services (NHPCO, 2015).
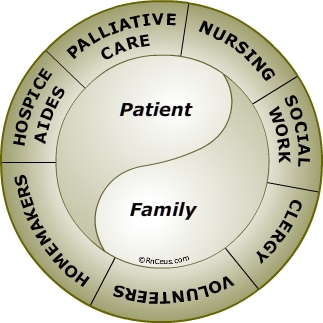
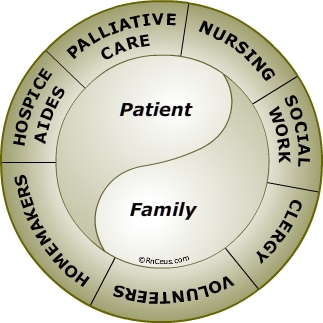
Hospice care team
Hospice care is provided by a coordinated team of health care professionals, caregivers and family/friends all focused on the comfort needs and care preferences of the patient. The health care team members communicate regularly to adjust the plan of care to meet the changing needs and preferences of the patient and to promote therapeutic family participation. Health care team professionals will usually include:
Hospice clients
Hospice is a program of care for the terminally ill patient, regardless of the type of illness. According to the National Hospice and Palliative Care Organization in 2014 a cancer diagnosis made up 36.6% of all patients in hospice programs. Non-cancer diagnoses were 63.4%. The most common non-cancer diagnoses were dementia (14.8%), heart disease (14.7%), lung disease (9.0%), and stroke or coma (6.4%). (http://www.nhpco.org/sites/default/files/public/Statistics_Research/2015_Facts_
Figures.pdf )
Hospice provides palliative care focused on management of symptoms caused by a terminal illness. Symptoms treated by palliative care can include: pain, nausea, GI upsets, excessive secretions and so forth. The patient care approach is on support and comfort, not on curing the terminal illness. The emphasis is caring for the ‘whole person’ including physical, emotional, social and spiritual care.
In a study by the Pew Research Center (2013) while 57% of adults would prefer to stop treatment so they could die if they had an incurable, painful disease, 35% would tell their doctors to do everything to save their lives. The remaining 8% were uncertain. It is important for health professionals to provide information about hospice while respecting the preferences of the patient.
When an illness has advanced beyond the possibility of a cure, research has shown that early enrollment in hospice care helps patient live longer with better quality of life (Connor, Pyenson, Fitch, Spence & Iwasaki, 2007). Other benefits include assistance for the family that may decrease complicated bereavement and increase preparation for the death of a loved one. Nilsson et al. (2011) found younger patients who were white, without a DNR order and in the ICU during the last week of life had the worse quality of life at the end of life. Patients who reached a feeling of inner peace and were cared for by an oncologist who saw them as a person were more likely to have a better quality of life.
Core Components of Quality End-of-Life Care
The Institute of Medicine (IOM, 2015) authors list the following as core components of quality end of-life care:
- Frequent assessment of the patient’s physical, emotional, social, and spiritual well-being
- Management of emotional distress
- Referral to expert-level palliative care
- Referral to hospice if the patient has a prognosis of 6 months or less
- Management of care and direct contact with patient and family for complex situations by a specialist- level palliative care physician
- Round-the-clock access to coordinated care and services
- Management of pain and other symptoms
- Counseling of patient and family
- Family caregiver support
- Attention to the patient’s social context and social needs
- Attention to the patient’s spiritual and religious needs
- Regular personalized revision of the care plan and access to services based on the changing needs of the patient and family
Hospice Quality Reporting
Section 3004 of the Patient Protection Affordable Care Act, 2010, requires that all Medicare certified hospices submit quality of care data to the Centers for Medicare and Medicaid Services (CMS). Hospice providers that fail to meet reporting requirements will receive a 2-percentage point reduction in reimbursement. The CMS uses this data to calculate quality compliance with measures endorsed by the National Quality Forum (NQF).
The current quality measures include:
- NQF #1617 Patients Treated with an Opioid who are Given a Bowel Regimen -
Percentage of vulnerable adults (including hospice patients) treated with an opioid that are offered/prescribed a bowel regimen or documentation of why this was not needed.
- NQF #1634 Pain Screening -
Percentage of hospice or palliative care patients who were screened for pain during the hospice admission evaluation / palliative care initial encounter.
- NQF #1637 Pain Assessment -
This quality measure is defined as the percentage of hospice or palliative care patients who screened positive for pain and who received a clinical assessment of pain within 24 hours of screening.
- NQF #1639 Dyspnea Screening -
Percentage of hospice or palliative care patients who were screened for dyspnea during the hospice admission evaluation / palliative care initial encounter.
- NQF #1638 Dyspnea Treatment -
Percentage of patients who screened positive for dyspnea who received treatment within 24 hours of screening.
- NQF #1641 Treatment Preferences -
Percentage of patients with chart documentation of preferences for life sustaining treatments.
- Modified NQF #1647 Beliefs/Values Addressed (if desired by the patient) -
This measure reflects the percentage of hospice patients with documentation of a discussion of spiritual/religious concerns or documentation that the patient/caregiver/family did not want to discuss.
References