 The three main functions of HIV testing are (1) screening of donated blood and organs, (2) epidemiological surveillance of HIV prevalence or trends and (3) diagnosis of infection in individuals.
The three main functions of HIV testing are (1) screening of donated blood and organs, (2) epidemiological surveillance of HIV prevalence or trends and (3) diagnosis of infection in individuals. The CDC reports that at least 50% of the new U.S. HIV cases are transmitted by acutely infected individuals who are unaware that they are infected. "The prevalence of high-risk sexual behavior is reduced substantially after people become aware they are HIV+."• Therefore, HIV testing is integral to preventing the transmission of HIV. HIV infection can be diagnosed by serologic tests that detect antibodies against HIV-1 and HIV-2 and by virologic tests that can detect HIV antigens or ribonucleic acid (RNA).
 The three main functions of HIV testing are (1) screening of donated blood and organs, (2) epidemiological surveillance of HIV prevalence or trends and (3) diagnosis of infection in individuals.
The three main functions of HIV testing are (1) screening of donated blood and organs, (2) epidemiological surveillance of HIV prevalence or trends and (3) diagnosis of infection in individuals.
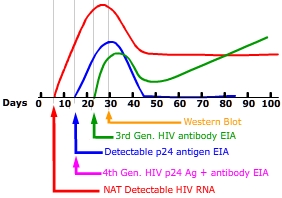
 HIV infected individuals present the greatest risk of transmission in the acute HIV infection (AHI) phase. During AHI, virus concentration rapidly increases in plasma and sexual fluids. The AHI phase begins 2-4 weeks after infection and continues until immune system rebounds as evidenced by a decline in HIV plasma concentration and increase in CD4+ counts. It is estimated that 50% of patients will seek medical care during AHI for symptoms resembling mononucleosis or influenza. The remainder of persons may have few to no symptoms.
HIV infected individuals present the greatest risk of transmission in the acute HIV infection (AHI) phase. During AHI, virus concentration rapidly increases in plasma and sexual fluids. The AHI phase begins 2-4 weeks after infection and continues until immune system rebounds as evidenced by a decline in HIV plasma concentration and increase in CD4+ counts. It is estimated that 50% of patients will seek medical care during AHI for symptoms resembling mononucleosis or influenza. The remainder of persons may have few to no symptoms.The FDA considers the sensitivity and a specificity of HIV tests when granting approval. A test with high sensitivity is one that can detect minute amounts of HIV antigen or antibodies and thus has a low level of false negative responses. A test with high specificity produces very few false positives. There are two main types of HIV tests approved for use in America. The majority of tests administered are enzyme-linked immunosorbent assays (ELISA or EIA), that detect HIV antibodies in the serum or plasma but some tests can use whole blood, dried bloodspots, oral transudate or urine. Tests that detect HIV nucleic acids like RNA and DNA are used on pooled samples by blood banks and in individual patients when antibodies may be very low, when antibody tests are indeterminate or when maternal HIV antibodies may cause a false positive in neonatal testing.
 Enzyme-linked immunosorbent assay (ELISA or EIA) is often the first test used to screen for HIV. 3rd EIAs technology begins with synthetic HIV proteins adhered to the bottom of assay wells. The wells are flooded with diluted patient plasma. Patient plasma antibodies produced in response to HIV infection bind to the HIV proteins at the bottom of the wells. Secondary antibodies and signalling enzyme are added that binds to the HIV antigen/patient antibody complex allowing it to be identified. If the test is negative a follow-up test may be done later if the patient is high risk or if testing could have occurred before adequate levels of antibodies were produced (window period).
Enzyme-linked immunosorbent assay (ELISA or EIA) is often the first test used to screen for HIV. 3rd EIAs technology begins with synthetic HIV proteins adhered to the bottom of assay wells. The wells are flooded with diluted patient plasma. Patient plasma antibodies produced in response to HIV infection bind to the HIV proteins at the bottom of the wells. Secondary antibodies and signalling enzyme are added that binds to the HIV antigen/patient antibody complex allowing it to be identified. If the test is negative a follow-up test may be done later if the patient is high risk or if testing could have occurred before adequate levels of antibodies were produced (window period).
 Western Blot was once the "gold standard" for HIV testing due to antibody specificity. The western blot detects antibodies to multiple specific HIV proteins. A western blot is considered negative if no antibodies bind to any of the specific test HIV proteins including: gp 160, gp120, p68, p55, gp41, gp41, p40, p34, p24, p17.
Western Blot was once the "gold standard" for HIV testing due to antibody specificity. The western blot detects antibodies to multiple specific HIV proteins. A western blot is considered negative if no antibodies bind to any of the specific test HIV proteins including: gp 160, gp120, p68, p55, gp41, gp41, p40, p34, p24, p17.| Specimen Type | Sensitivity | Specificity | Approved for HIV-2 | Read time | |
| OraQuick In-Home HIV-1/2 Test (OTC) | Oral fluid | 92% | 99.8% | Yes | 20-40 |
| OraQuick ADVANCE Rapid HIV-1/2 Antibody Test | Oral fluid | 99.3% | 99.8% | Yes | 20-40 minutes |
| Whole blood (venipuncture or finger stick | 99.6% | 100% | |||
| Plasma | 99.6% | 99.9% | |||
| Uni-Gold Recombigen HIV | Whole blood (finger stick or venipuncture) |
100% | 99.7 | No | 10-12 minutes |
| Serum & Plasma | 100% | 99.8% | |||
| Reveal G-3 Rapid HIV-1 Antibody Test | Serum | 99.8% | 99.1% | No | Read immediately |
| Plasma | 99.8% | 98.6% | |||
| MultiSpot HIV-1/HIV-2 Rapid Test | Serum | 100% | 99.93% | Yes - differentiates between HIV-1 and HIV-2 | Read immediately or up to 24 hrs |
| Plasma | 100% | 99.91% | |||
| Clearview HIV 1/2 STAT-PAK | Whole blood (venipuncture or finger stick | 99.7% | 99.9% | Yes | 15-20 minutes |
| Serum & Plasma | 99.7% | 99.9% | |||
| Clearview COMPLETE HIV 1/2 | Whole blood (venipuncture or finger stick | 99.7% | 99.9% | Yes | 15-20 minutes |
| Serum & Plasma | 99.7% | 99.9% |
Tests used to stage the disease or to evaluate the effectiveness of treatment include:
CD4+ cells aka Helper T cells are a subset of lymphocytes. CD4+ lymphocytes aren't phagocytic or cytotoxic, rather they activate other immune cells. When a specialized cell like an epithelial Langerhans cell captures an antigen, it migrates to the lymphatic system. In the lymphatic system the dendritic cell presents a processed portion of the antigen to a Helper T cells. The dendritic cell/antigen complex activates Helper T cells to secrete chemicals called lymphokines. These lymphokines stimulate cytotoxic T cells and B cells to grow and divide, attract neutrophils, and enhance the ability of macrophages to engulf and destroy microbes. HIV progressively destroys CD4+ cells as a result of viral reproduction. Loss of Helper T cells derails the immune response.
|
Test |
Normal
results |
CDC Classification System for HIV-Infected Adults and Adolescents |
|||
| CD4 lymphocyte count | 500-1500 cells/µL |
CD4 Categories |
Asymptomatic |
Symptomatic |
AIDS Indicator |
| (1) ≥500 cells/µL | A1 |
B1 |
C1 |
||
| (2) 200-499 cells/µL | A2 |
B2 |
C2 |
||
| (3) <200 cells/µL | A3 |
B3 |
C3 |
||
| CD4 percentage | CD4 Percentage is a comparison of the number of CD4 cells to the total lymphocyte count (B- and T-lymphocytes). The CD4 percentage may be a more accurate measure of HIV disease progression than the CD4 count, because immune suppression may be present despite a high CD4 count. A CD4 percentage below 20% suggests serious immune deficiency, even if the CD4 count is high. |
Viral load
The viral load indicates the number of copies of HIV in the blood. Viral load in conjunction with CD4 results provide an indication of disease stage and the effectiveness of treatment. The higher viral load the greater the risk for immune system damage that in turns leaves the body at risk for opportunistic infections.
HIV viral load may be measured by assays such as:
A non-detectable result does not mean that there is no virus present; just that it was not detected. The newer versions of tests can now detect a load as few as 5 copies and as high as 1.5 million. A level of 55,000 requires antiretroviral treatment. Antiretroviral treatment is considered to be working if viral load drops by 90% within 8 weeks and continues to drop to less than 50 copies within 6 months. Different tests that give slightly different results. Therefore, when possible, people should be tested consistently with the same type of test.
HIV Phenotypic and Genotypic Testing
HIV's rapid mutation rate, rapid reproductive rate, and enormous population size eventually results in antiretroviral resistance. Phenotypic susceptibility testing assesses the ability of specific drugs or drug combinations to inhibit viral replication in cultured cells. Genotypic testing assesses the genetic composition of HIV variants in infected individuals to determine precisely which resistance mutations they carry.