Fall Prevention Programs
In the section entitled fall risk factors, we identified intrinsic patient risk factors for falls that need to be assessed during the beginning of the throughput phase - the admission to a hospital. We also described some of the hospital environmental factors and extrinsic patient factors such as medications in the throughput phase that increase the risk of falls. In this section we will be describing the components of fall prevention programs that address these risk factors to reduce falls as well as recommendations by organizations that require fall prevention programs.
The Joint Commission (TJC) Requirements for a fall prevention program
The Joint Commission (TJC) requires accredited health care organizations to implement a falls reduction program and to conduct an evaluation of the effectiveness of that program. Here are their standards of care requirements related to falls.
Hospital standards directly related to fall prevention Performance Improvement (PI)
PI.01.01.01 EP 38: The hospital evaluates the effectiveness of all fall reduction activities including assessment, interventions, and education. Note: Examples of outcome indicators to use in the evaluation include number of falls and number and severity of fall-related injuries.
Provision of Care, Treatment, and Services (PC)
PC.01.02.08: The hospital assesses and manages the patient's risk for falls. EP 1: The hospital assesses the patient's risk for falls based on the patient population and setting. EP 2: The hospital implements interventions to reduce falls based on the patient's assessed risk http://www.jointcommission.org/assets/1/18/SEA_55.pdf
Medicare, Medicaid and other payers
As mentioned in the background section of this course, Medicare and other payers require detailed reporting of all falls that occur in hospitals. They do not recommend a specific fall prevention program. Other government agencies and organizations provide detailed descriptions of fall prevention programs.
The National Council on Aging and the Center for Healthy Aging
The National Council on Aging and the Center for Healthy Aging originated a falls free initiative promoting state legislation and funding in some circumstances to reduce falls in the elderly in all community places, including hospitals. These initiatives vary from state to state. Many states have legislation that requires education of health professionals in fall prevention. Here, for example, is the initiative for fall reduction in Massachusetts.
Since medication is a risk factor for falls, an annual medication review program and appropriate modifications can be made a requirement of state prescription drug programs and can be expanded to other insurance plans (Massachusetts Department of Public Health, 2008). In response to the CMS decision not to reimburse hospitals on the medical costs of a fall-related injury occurring within the facility, the Massachusetts Department of Public Health introduced regulations that require hospitals to develop strategic plans to reduce falls in hospital settings (p. 13-14).
Here is one example of how this initiative promoted education of medical students.
North Carolina
The University of North Carolina at Chapel Hill's School of Medicine requires all third year medical students to complete a training unit on falls risks and prevention, and to pass a skills exam for conducting falls risk assessments for older adults. The School of Medicine is in the process of piloting a complex geriatric case that focuses on falls risk. All medical students must successfully pass the geriatric case exam to begin their fourth year of study. As a result, several of the residency programs at the UNC School of Medicine, including family practice and physical medicine and rehabilitation, are also incorporating falls evaluation and prevention training modules (p.21).
It is recommended as part of this course to read this initiative with particular attention to legislation in your state about falls prevention. http://www.homesafety.net/Portals/4/Resources/State_Fall_Prevention_Legislative _and_Policy_Initiatives.pdf
 Agency for Healthcare Research and Quality (AHRQ)
Agency for Healthcare Research and Quality (AHRQ)
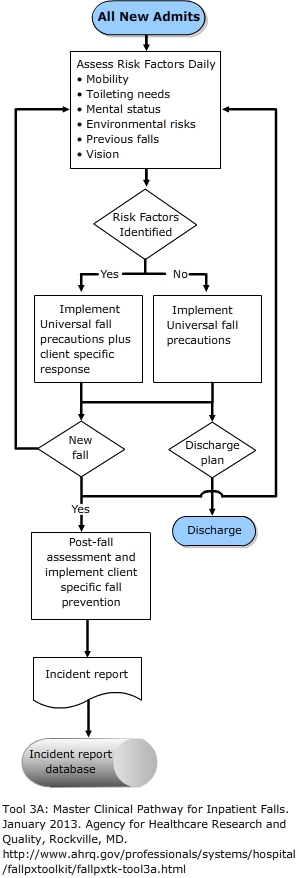
The Agency for Healthcare Research and Quality (AHRQ) with a core team of experts in fall prevention from the RAND Corporation, ECRI Institute, and Boston University created a detailed toolkit for a fall prevention program for hospitals. In this report, it is recommended fall prevention activities be broken down into the following steps:
The AHRQ also reinforces the approach that fall prevention practices be tailored to the specific hospital and patient needs. This report includes a warning also that fall prevention must be considered as a part of good quality patient care. It must be balanced with the patients need for ambulation to maintain muscle strength and avoid deconditioning. Restraints and sedation, for example, are sometimes believed to prevent falls but in fact can increase serious fall injuries and lead to complication of bedrest (Ganz, et al., 2013).
This AHRQ report is a comprehensive description of all aspects of fall prevention program. It includes also a falls clinical pathway as described below. It is recommended as part of this course to read through this report. http://www.ahrq.gov/professionals/systems/hospital/fallpxtoolkit/fallpxtkover.html
Instant feedback
Specific fall prevention recommendations
Rand Health (Hempel et al., 2012) published a "Review of the Evidence on Falls Prevention in Hospitals". The review is a systematic literature search and analysis of interventions intended to prevent falls in hospitals. The literature search returned 2473 publications. Using the following 3 criteria, Rand Health categorized 102 studies published over 30 years:
Analysis of the Rand report
The standard goal for hospitals has been to reduce the fall rate to 3 per 1000 patient days. Most hospitals reporting success in reducing the number of falls per patient days were able to achieve that goal with one reducing their fall rate to 1.37 per 1000 days (Gutierrez et al., 2008). Since some hospitals are able to reduce the fall risk below 2 per 1000 patient days, the goal of the fall prevention program in a hospital should be to reduce the risk to 1 per 1000 patient days instead of 3, setting the goal appropriately just beyond the current reach.
The basic components of the successful fall programs analyzed in the RAND studies have been
Example of a fall prevention program
Krauss et al. (2008) studied fall rates in 4 general medicine floors in a 1300 bed tertiary care academic hospitals. There were 135 patients in the intervention group and 78 patients in the control group. The intervention group received the following interventions:
The control group received the usual care which included: daily risk assessment, pt / family education, signs, other measures. The results showed a statistically significant difference between the rate of falls in the intervention group before and after the intervention. A rate of 6.84 was reduced to 3.81 falls per 1000 patient days at the 5 month interval. However, the change did not remain after 9 months.
Hawthorne Effect
Many of the studies reported the positive effects of the interventions tapering off after a few months. This may represent the Hawthorne Effect, where staff altered behavior as a result of participating in a study.
It is important that the issue of fall prevention be continuously reinforced. The three month progress report of falls, used in many hospitals, is too long an interval to provide continuous reinforcement. Each unit should display a weekly fall report of their unit. This is one of the most valuable variables for reducing falls.
Instant feedback
References
RnCeus.com