Insulin
Regimens
The goal of insulin therapy
is to achieve optimal blood glucose control. Healthy, non-diabetic individuals usually maintain a blood glucose profile of 60 – 100 mg/dl overnight and before meals, and <140 mg/dl after meals. Specific blood glucose levels for diabetics are controversial but health providers often recommend overnight and pre-meal blood glucose of <90-130 mg/dl and post-meal blood glucose of <180 mg/dl.•
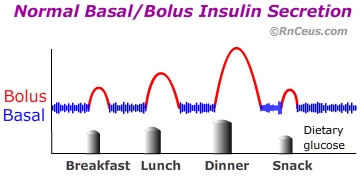 Normally the pancreas secretes insulin in response to blood glucose levels. Pancreatic beta cells continuously release a small amount of insulin into the blood stream. Additional insulin is released in response to a rise in blood glucose that occurs after eating. The
continuous release of insulin is known as basal secretion. Insulin released
in response to an increase in blood sugar is known as bolus secretion.
Normally the pancreas secretes insulin in response to blood glucose levels. Pancreatic beta cells continuously release a small amount of insulin into the blood stream. Additional insulin is released in response to a rise in blood glucose that occurs after eating. The
continuous release of insulin is known as basal secretion. Insulin released
in response to an increase in blood sugar is known as bolus secretion.
An individual's basal insulin requirement can vary due
to physical stress, hormonal changes, physical activity, and over all health. Effective insulin regimens are individualized to reflect the patient's health, goals, lifestyle and ability for self-management. Designing an effective insulin regimen involves working
with the patient to select a regimen that provides adequate insulin coverage and flexibility
in regard to calorie intake, mealtime, physical activity, work schedule, other medications, psychosocial
and economic factors.
The insulin requirements of diabetic patients reflect the underlying disease.
- Type 1 diabetes (T1D) is the result of the complete or near complete absence of endogenous insulin secretion. Treatment involves replacing endogenous insulin secretion. In other
words, optimum insulin delivery must provide continuous basal release with additional preprandial boluses reflecting the size and type of meals consumed. Basal insulin requirements may vary due
to physical stress, hormonal changes, illness, physical activity, and level
of physical fitness. Designing an effective insulin regimen involves working
with the patient to develop a program that provides adequate insulin coverage and schedule flexibility.
- T2D is characterized by progressive insulin resistance, decreased insulin secretion, and decreased suppression of hepatic glucose production. Initially, T2D is usually treated by lifestyle modification and oral agents like metaformin, however, less than 40% of T2D patients are able to maintain an A1C of <7. Progressive beta cell failure often requires the addition of insulin therapy to avoid prolonged hyperglycemia which can cause glucose toxicity, a potentially reversible impairment in glucose-stimulated insulin secretion.•
Historically, insulin therapy for (T1D) required serial injections of short duration insulin throughout the day. This type of regimen resulted in an increased risk of hypoglycemic events, patient discomfort and non-compliance. The advent of intermediate duration neutral protamine hagedorn (NPH) insulin, named for Hans Christian Hagedorn, and self-monitoring blood glucose improved blood glucose control for many T1D patients.
Today, rapid and accurate self-monitoring blood glucose devices in conjunction with insulins with various onsets and durations of action offer diabetics much better glycemic control. Currently, ultra-rapid acting, rapid-acting, (regular) short duration, NPH intermediate duration and long duration forms of insulin, as well as premixed combination preparations are FDA approved for use.
Over the past few years,
research has shown that tight control of blood sugar reduces
the microvascular complications of diabetes. Intensive therapy utilizing long duration insulin and multiple rapid or short duration insulin
injections throughout the day is improving A1C for T1D patients. Studies
have shown that 3 or 4 injections a day provide the best blood sugar control
and reduce or delay eye, kidney, and nerve damage caused by diabetes. Intensive
insulin therapy allows better insulin coverage, reducing the risk of nighttime
hypoglycemia and morning hyperglycemia, the latter due to the normal release
of cortisol and growth hormone early in the day.
For most patients with T1D, achieving adequate blood glucose control requires using intensive
therapy. With a 3 injection regimen, insulin is injected in the morning before
breakfast, before the evening meal, and at bedtime, or before each meal. A 4 injection regimen involves insulin is injections in the morning before breakfast,
before lunch, before the evening meal, and at bedtime.
Once-daily insulin regimens may be useful for patients that are: a) poorly controlled T2D, b) unable to implement more complicated regimens, i.e., (poorly motivated patients or disable patients).
Instant
Feedback:
Intensive
insulin therapy involves injecting insulin once in the morning and at bedtime.
Insulin regimens for
T1D or T2D patients, incorporate the individual’s insulin deficiency, insulin resistance, comorbidities, lifestyle and socio-economic factors. Insulin requirements
for persons with T1D, who are within 20% of ideal body weight, range
between one half and 1 unit per kilogram of body weight per day. During illness,
insulin requirements rise for persons with either T1D or T2D,
sometimes to several hundred units per day, depending on the extent of insulin
deficiency and resistance. Insulin requirements for pregnant women with pre-existing
diabetes gradually increase during the second and third trimesters of pregnancy.
Instant
Feedback:
Insulin
requirements for pregnant women with pre-existing diabetes gradually decrease
during the 2nd and 3rd trimesters of pregnancy.
Once-daily insulin regimen (Basal)(T2D)
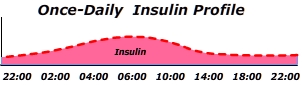 This regimen is often used to transition T2D patients to insulin therapy when oral agents alone fail to maintain blood glucose targets. Once-daily involves the administration of a single dose of a long-acting insulin analog or NPH insulin. This single dose provides enough basal insulin to suppress hepatic glucose production with little risk of hypoglycemia. "Using a single dose of basal insulin in those with type 2 diabetes initiating insulin will result in good glycemic control in about 70% of patients, with a low percentage (about 30-40%) of patients experiencing a few (about 6) episodes of mild hypoglycemia per year."•
This regimen is often used to transition T2D patients to insulin therapy when oral agents alone fail to maintain blood glucose targets. Once-daily involves the administration of a single dose of a long-acting insulin analog or NPH insulin. This single dose provides enough basal insulin to suppress hepatic glucose production with little risk of hypoglycemia. "Using a single dose of basal insulin in those with type 2 diabetes initiating insulin will result in good glycemic control in about 70% of patients, with a low percentage (about 30-40%) of patients experiencing a few (about 6) episodes of mild hypoglycemia per year."•
Gluconeogenesis occurring in the overnight fasted state is responsible for approximately two thirds of hepatic glucose production in T2D subjects and results in about 5% to 10% increased blood glucose compared to healthy subjects. Some experts suggest initiating insulin therapy when fasting blood glucose level is consistently greater than 250 mg per dL (13.90 mmol per L), or if random testing shows levels greater than 300 mg per dL.•
Twice-daily Insulin (Bi-phasic)(T1D)
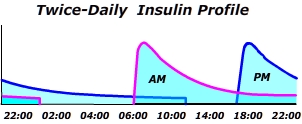 Once daily insulin is convenient but it fails to control dietary glucose increases. Twice-daily regimens incorporating a 30/70% mixture of short-acting and long-acting analog insulins, respectively, provides better glucose control. "Using mix-insulin twice daily before breakfast and dinner has the advantage that it provides both 24-hour basal insulinemia and meal-related insulin substitution for two meals. Although insulin 30/70% premixes of Regular insulin/NPH insulin are being replaced by more modern rapid-acting analog/intermediate duration analog mixtures, an advantage has not been demonstrated by the later •
Once daily insulin is convenient but it fails to control dietary glucose increases. Twice-daily regimens incorporating a 30/70% mixture of short-acting and long-acting analog insulins, respectively, provides better glucose control. "Using mix-insulin twice daily before breakfast and dinner has the advantage that it provides both 24-hour basal insulinemia and meal-related insulin substitution for two meals. Although insulin 30/70% premixes of Regular insulin/NPH insulin are being replaced by more modern rapid-acting analog/intermediate duration analog mixtures, an advantage has not been demonstrated by the later •
- A twice daily regimen in T1D may be suitable if someone has a regular daily routine that includes three main meals at similar times each day.
- A twice daily regimen may be appropriate for T1D school children as injections can be given before and after school without the need for an injection during lunch.
- A twice daily insulin regimen may be recommended for people with T2D who experience significantly high blood glucose levels after eating.•
Intensive (Basal/Bolus) Therapy
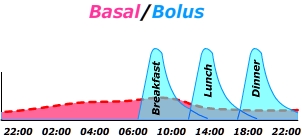 This type of insulin therapy attempts to closely approximate the normal physiologic condition of continuous low level insulinemia with steep short duration insulin boluses to cover dietary glucose at mealtimes. The Basal/Bolus diagram on the right demonstrates a common injection pattern, beginning with an initial injection of long duration "peakless" analog insulin administered around 22:00. The initial dose is followed by a dose of rapid acting/short duration analog delivered at each mealtime. Basal/Bolus regimens offer a bit more flexibility but they require more attention to blood glucose monitoring and active self adjustment of bolus dosing
This type of insulin therapy attempts to closely approximate the normal physiologic condition of continuous low level insulinemia with steep short duration insulin boluses to cover dietary glucose at mealtimes. The Basal/Bolus diagram on the right demonstrates a common injection pattern, beginning with an initial injection of long duration "peakless" analog insulin administered around 22:00. The initial dose is followed by a dose of rapid acting/short duration analog delivered at each mealtime. Basal/Bolus regimens offer a bit more flexibility but they require more attention to blood glucose monitoring and active self adjustment of bolus dosing
Instant
Feedback:
Which form of diabetes is characterized by complete or near complete loss of beta cell secretion of insulin?
©RnCeus.com
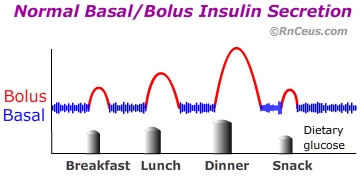 Normally the pancreas secretes insulin in response to blood glucose levels. Pancreatic beta cells continuously release a small amount of insulin into the blood stream. Additional insulin is released in response to a rise in blood glucose that occurs after eating. The
continuous release of insulin is known as basal secretion. Insulin released
in response to an increase in blood sugar is known as bolus secretion.
Normally the pancreas secretes insulin in response to blood glucose levels. Pancreatic beta cells continuously release a small amount of insulin into the blood stream. Additional insulin is released in response to a rise in blood glucose that occurs after eating. The
continuous release of insulin is known as basal secretion. Insulin released
in response to an increase in blood sugar is known as bolus secretion.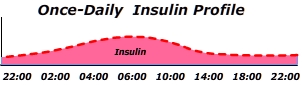 This regimen is often used to transition T2D patients to insulin therapy when oral agents alone fail to maintain blood glucose targets. Once-daily involves the administration of a single dose of a long-acting insulin analog or NPH insulin. This single dose provides enough basal insulin to suppress hepatic glucose production with little risk of hypoglycemia. "Using a single dose of basal insulin in those with type 2 diabetes initiating insulin will result in good glycemic control in about 70% of patients, with a low percentage (about 30-40%) of patients experiencing a few (about 6) episodes of mild hypoglycemia per year."
This regimen is often used to transition T2D patients to insulin therapy when oral agents alone fail to maintain blood glucose targets. Once-daily involves the administration of a single dose of a long-acting insulin analog or NPH insulin. This single dose provides enough basal insulin to suppress hepatic glucose production with little risk of hypoglycemia. "Using a single dose of basal insulin in those with type 2 diabetes initiating insulin will result in good glycemic control in about 70% of patients, with a low percentage (about 30-40%) of patients experiencing a few (about 6) episodes of mild hypoglycemia per year."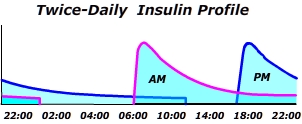 Once daily insulin is convenient but it fails to control dietary glucose increases. Twice-daily regimens incorporating a 30/70% mixture of short-acting and long-acting analog insulins, respectively, provides better glucose control. "Using mix-insulin twice daily before breakfast and dinner has the advantage that it provides both 24-hour basal insulinemia and meal-related insulin substitution for two meals. Although insulin 30/70% premixes of Regular insulin/NPH insulin are being replaced by more modern rapid-acting analog/intermediate duration analog mixtures, an advantage has not been demonstrated by the later
Once daily insulin is convenient but it fails to control dietary glucose increases. Twice-daily regimens incorporating a 30/70% mixture of short-acting and long-acting analog insulins, respectively, provides better glucose control. "Using mix-insulin twice daily before breakfast and dinner has the advantage that it provides both 24-hour basal insulinemia and meal-related insulin substitution for two meals. Although insulin 30/70% premixes of Regular insulin/NPH insulin are being replaced by more modern rapid-acting analog/intermediate duration analog mixtures, an advantage has not been demonstrated by the later 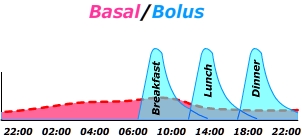 This type of insulin therapy attempts to closely approximate the normal physiologic condition of continuous low level insulinemia with steep short duration insulin boluses to cover dietary glucose at mealtimes. The Basal/Bolus diagram on the right demonstrates a common injection pattern, beginning with an initial injection of long duration "peakless" analog insulin administered around 22:00. The initial dose is followed by a dose of rapid acting/short duration analog delivered at each mealtime. Basal/Bolus regimens offer a bit more flexibility but they require more attention to blood glucose monitoring and active self adjustment of bolus dosing
This type of insulin therapy attempts to closely approximate the normal physiologic condition of continuous low level insulinemia with steep short duration insulin boluses to cover dietary glucose at mealtimes. The Basal/Bolus diagram on the right demonstrates a common injection pattern, beginning with an initial injection of long duration "peakless" analog insulin administered around 22:00. The initial dose is followed by a dose of rapid acting/short duration analog delivered at each mealtime. Basal/Bolus regimens offer a bit more flexibility but they require more attention to blood glucose monitoring and active self adjustment of bolus dosing