Insulin
Administration
For insulin therapy to be
safe and effective, patient adherence to specific preparation and injection routines is required. Patient education should include product specific storage, injection technique, accurate dosages,
and site rotation.
 Storage:•
Storage:•
- Store insulin according
to the manufacturer's instructions.
- Check storage guidelines specific to the insulin formulation. (usually in the product package insert).
- When ordering insulin through the mail, verify that the insulin will be shipped under proper conditions.
- Never freeze insulin. (Frozen insulin should be thrown away.)
- Never use insulin beyond the expiration date stamped by the drug manufacturer on the vial, pen, or cartridge.
- Avoid exposing insulin to direct heat, light or excessive agitation. The longer the exposure to extremes, the less effective the insulin becomes.
- Unopened, not-in-use insulin should be stored in a refrigerator at a temperature of 36-46o F and should retain potency until the expiration date.
- Opened, in-use insulin should be stored at room temperature 59-86o F for up to 28 days.
- Pre-filling and storage of insulin syringes by patients is not recommended by some insulin manufacturers (check the product insert label) If allowed, store syringes with the needle pointing up to avoid obstruction of needle lumen. One study indicated that the qualities of the disposable syringe significantly effected the stability and efficacy of Lantus® insulin over a seven day period.•
- Examine vials of liquid insulin
for sediment or other visible changes.
- Regular insulin,
lispro, aspart, and glargine are clear insulins.
- All other types of
insulin are suspensions with a milky appearance.
- A clear insulin preparation
that becomes cloudy or discolored or an insulin suspension that shows clumping
or has a frosty appearance indicates that the insulin may be contaminated or has lost potency
and should be discarded or returned to the pharmacy.
- Patient prepared prefilled syringes should be labeled, refrigerated and used within 14 days.
Education:
- Newly diagnosed patients will benefit from patient education and learning tools.
- Stress the importance of:
- injection site selection
- skin preparation
- medication handling
- verification of expirations dates
- When mixing two types
of insulin
in a single syringe
- rapid-acting or regular insulin is drawn up first, followed by
the longer acting insulin.
- insulins to be mixed should be of the same commercial brand.
- Commercially prepared insulin mixtures are accurate, stabilized and convenient which may improve safety, compliance and benefit the patient.
Injection:
 Insulin is rapidly broken down
in the gastrointestinal tract, it cannot be taken orally. Therefore, insulin medications must be administered parenterally, with the exception of Afrezza®, which must be inhaled.
Insulin is rapidly broken down
in the gastrointestinal tract, it cannot be taken orally. Therefore, insulin medications must be administered parenterally, with the exception of Afrezza®, which must be inhaled.
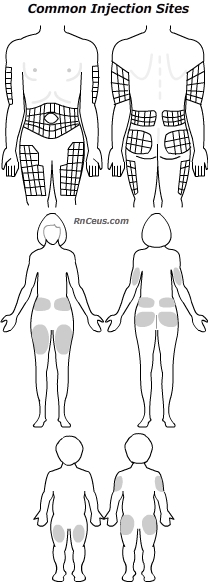
When injected, insulin should be delivered into the deep subcutaneous fat. It is recommended that the same anatomical area be used for injections given at the same time of day. The exact site should be changed systematically to utilize the entire area. In type-1 adults, the abdominal wall is the preferred site for mealtime injections. An extended profile of action can be obtained when type-1 adults inject long acting suspensions like NPH in the thigh rather than the arm or abdominal wall.
There are a variety of insulin delivery devices available today. The typical device is a disposable U-100 syringe and needle. Syringe sizes range from .25cc to 1cc. Needle length can be 5/16 or 1/2 inch. Selection of needle length should be based upon injection site. Needle angle should enter the skin at 90o for adults and 45o for thin adults and children.
Optimal compliance with the ordered insulin regimen may require more than one type of delivery device. Alternatives to the needle and syringe include:
- automatic syringe & needle injectors
- pen injectors
- needle-free jet injectors
- insulin pumps
Device appropriate disposal containers are part of a complete insulin regimen.
Instant
Feedback:
When
mixing insulins, the longer acting insulin preparation should be drawn up first
into the syringe.
Instant
Feedback:
The
place on the body where insulin is injected affects insulin absorption.
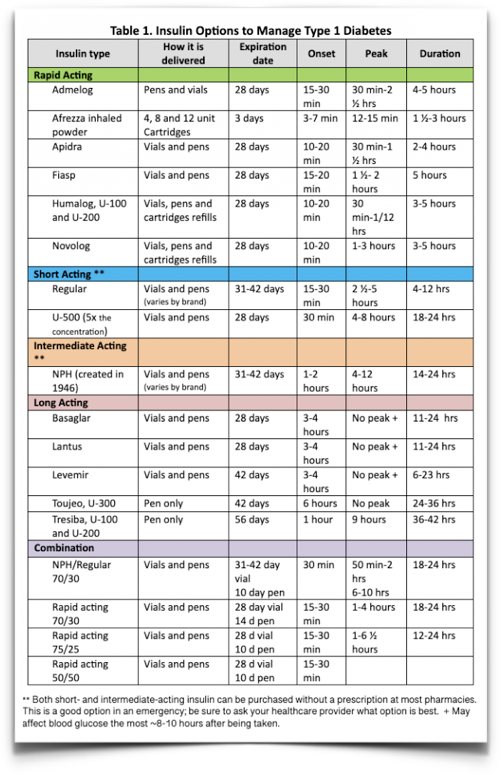
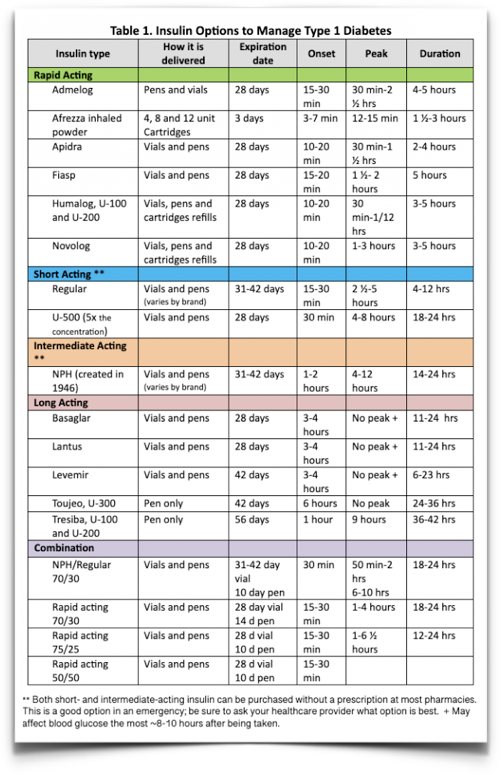
Reference
Table 1. Hess-Fischl, A & Smith-Marsh D.E. (2020). Insulin Options to Manage T1DM.
https://www.endocrineweb.com/conditions/type-1-diabetes/type-1-diabetes-treatments
©RnCeus.com
 Storage:•
Storage:•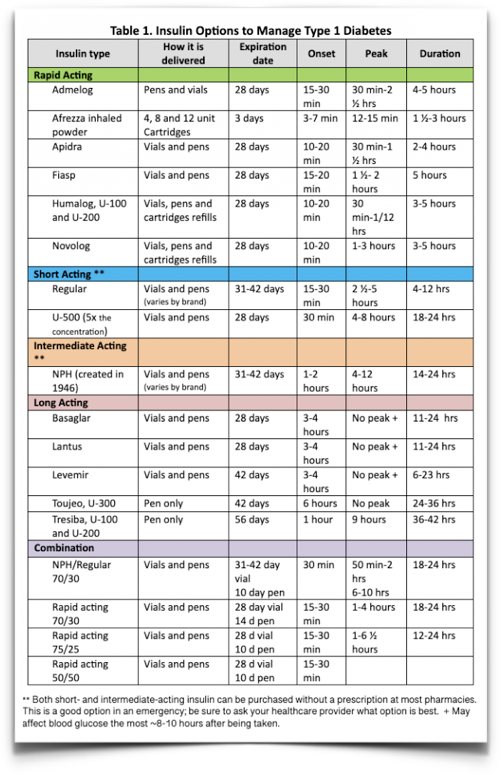 Storage:•
Storage:•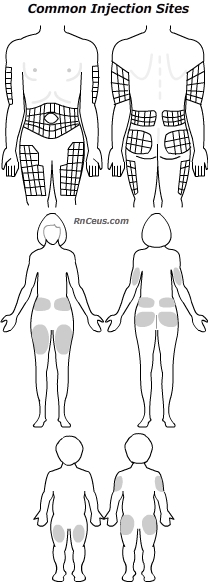 Insulin is rapidly broken down
in the gastrointestinal tract, it cannot be taken orally. Therefore, insulin medications must be administered parenterally, with the exception of Afrezza®, which must be inhaled.
Insulin is rapidly broken down
in the gastrointestinal tract, it cannot be taken orally. Therefore, insulin medications must be administered parenterally, with the exception of Afrezza®, which must be inhaled.