Anthrax
Background and potential
as a bioweapon
Anthrax is
one of the oldest infectious disease recorded in history. It is thought that
descriptions of plagues in the Bible’s book of Exodus may have been outbreaks
of anthrax in cattle and humans. Although anthrax spores distributed through
the U.S. mail were responsible for several deaths in the fall of 2001, a large
aerosol release of anthrax is a more significant threat to the U.S. population.
A World Health Organization (WHO) report estimated that 3 days after the release
of 50 kg of anthrax spores upwind of a city of 500,000 people, 125,000 infections
would occur, producing 95,000 deaths. It has also been estimated that an aerial
release of anthrax spores under ideal weather conditions could produce 50% mortality
rates as far as 100 miles downwind of the initial release point. A large exposure
of the population to anthrax would also have a huge economic impact. For each
100,000 persons exposed, it is estimated that $26.2 billion would be spent.
Epidemiology
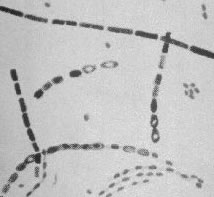 Anthrax is caused by infection with Bacillus anthracis, a gram-positive
spore-forming rod. The spore form of anthrax can survive in the environment
for many decades. Anthrax spores can be distributed in an aerosol form and are
quite resistant to environmental degradation. Anthrax spores from 2 to 6 microns
in size are the ideal size for infecting the mucosal surfaces of the lower respiratory
tract. Manufacturing and distributing anthrax spores in this size range, while
avoiding clumping together of larger spore particles, is one of the challenges
facing bioterrorists attempting to use anthrax as a weapon of mass destruction.
Both bacilli rods and spores are shown in this picture.
Anthrax is caused by infection with Bacillus anthracis, a gram-positive
spore-forming rod. The spore form of anthrax can survive in the environment
for many decades. Anthrax spores can be distributed in an aerosol form and are
quite resistant to environmental degradation. Anthrax spores from 2 to 6 microns
in size are the ideal size for infecting the mucosal surfaces of the lower respiratory
tract. Manufacturing and distributing anthrax spores in this size range, while
avoiding clumping together of larger spore particles, is one of the challenges
facing bioterrorists attempting to use anthrax as a weapon of mass destruction.
Both bacilli rods and spores are shown in this picture.
 Human anthrax
has three major clinical forms: cutaneous anthrax, inhalation anthrax, and gastrointestinal
anthrax. Cutaneous anthrax occurs when the bacillus is introduced through the
skin; inhalation anthrax, through the respiratory tract; and gastrointestinal
anthrax, by ingestion. Most anthrax cases are cutaneous forms of the disease.
Human anthrax
has three major clinical forms: cutaneous anthrax, inhalation anthrax, and gastrointestinal
anthrax. Cutaneous anthrax occurs when the bacillus is introduced through the
skin; inhalation anthrax, through the respiratory tract; and gastrointestinal
anthrax, by ingestion. Most anthrax cases are cutaneous forms of the disease.
In the USA, prior to the
2001 terrorist attack, most individuals contracted cutaneous anthrax by close
contact with products derived from infected cattle, sheep, and goats, such as
animal hides, hair, wool, bone, and meat. Cutaneous anthrax is easily recognizable,
and can be successfully treated with a number of antibiotics. If treated, cutaneous
anthrax is rarely fatal.
In contrast, the 2001 terrorist
attack utilized highly refined anthrax spores. The spores were intentionally
produced to maximize their pulmonary dispersion. This is done by reducing the
size of the spore particles. The smaller the particles the greater the number
and the deeper they can travel into the lungs.
Unrecognized or untreated
anthrax in all forms can lead to septicemia and death. Patients with gastrointestinal
anthrax have a mortality rate between 25% and 75%. As a potential weapon of
mass destruction, anthrax would likely be delivered in an aerosolized form,
causing inhalation anthrax. Case fatality rates for inhalational anthrax are
between 90% and 100%.
INSTANT
FEEDBACK:
The
gastrointestinal form of anthrax has the highest mortality rate.
Clinical course
Symptoms of
inhalational anthrax generally occur after an incubation period ranging between
1 and 6 days. After the incubation period, a nonspecific flu like illness occurs,
with symptoms of fever, myalgia or muscle aches, headache, a non-productive
cough, and mild chest discomfort. Often, a brief intervening period of improvement
follows the initial symptoms, followed by rapid deterioration. High fever, difficulty
breathing, cyanosis, and shock characterize this next phase. Death is universal
in untreated cases and may occur in as many as 100% of treated cases if therapy
is started more than 48 hours after symptoms begin. A large number of gram-positive
bacilli in nasal swabs or in environmental samples can help confirm a diagnosis
of anthrax where intentional release is suspected.

4th day of incubation
Widened mediastinum with infiltrates
|

13th day of incubation.
Mediastinum
continues to widen and infiltrates expand
|
Differentiating inhalational
anthrax from influenza-like illnesses is a diagnostic challenge, especially
during winter months when outbreaks of influenza are common. In the current
climate of threat to the U.S., emergency department personnel and primary care
physicians should maintain a high index of suspicion for inhalational anthrax.
Complicating the diagnosis is the fact that patients initially may not appear
very ill. The classic chest X-ray finding of a widened mediastinum or the development
of pleural effusions may be subtle or absent on initial medical evaluation.
A careful history, with assessment of specific risk factors, such as postal
worker, contact with livestock or animal products, laboratory exposure should
be obtained from patients with influenza type symptoms.
INSTANT
FEEDBACK:
Patients
with inhalation anthrax have an initial period of improvement, followed by
rapid deterioration.
Disease management
| Considerations: Person-to-person cutaneous anthrax is very
rare and person-to person pulmonary anthrax has never been reported. Nonetheless,
in a mass exposure both contact and droplet precautions should be considered.
Contact and droplet precautions may reduce the number of spores to which
caregivers are directly exposed. It is estimated that current known strains
of B. anthracis require the delivery of at least 8,000 spores to
produce pulmonary disease. Due to potentially incomplete decontamination,
the number of pulmonary victims and possibility of emergent invasive procedures,
it is conceivable that a hospital based caregiver could exceed that spore
count while delivering care during a mass exposure. Furthermore, even though
medical personnel would likely receive prophylatic vaccine and antibiotics
against known strains, weapons grade anthrax which has been bioengineered
to resist antibiotics may be available to terrorists. |
Ciprofloxacin, doxycycline,
and other antibiotics including tetracyclines, are used to treat anthrax. Keys
to successful management appear to be early institution of antibiotics and aggressive
supportive care. Chest tube draining of the recurring pleural effusions, which
are typically hemorrhagic, often lead to dramatic clinical improvement. Because
these effusions tend to build up again rapidly, maintaing the chest tube may
be beneficial.
Anthrax vaccine for pre-exposure
prophylaxis may be given to those at risk of exposure, such as members of the
U.S. military. First responders and medical personnel may be offered the vaccine
and/or prophylactic antibiotics. Post-exposure prophylaxis should be used for
persons who have been exposed to anthrax spores. The Food and Drug Administration
(FDA) has approved ciprofloxacin, doxycycline, and penicillin G procaine for
prophylaxis of inhalational anthrax. The optimum length of prophylaxis is uncertain,
however, 60 days is recommended, primarily on the basis of animal studies of
anthrax deaths. In December 2001, the Department of Health and Human Services
(DHHS) announced additional options for prophylaxis against inhalational anthrax
for persons who wish to take extra precautions, especially for those whose exposure
was high. Three options are now offered: 1) 60 days of antibiotic prophylaxis;
2) 100 days of antibiotic prophylaxis, and 3) 100 days of antibiotic prophylaxis,
plus anthrax vaccine. Even though, under normal conditions, Anthrax has little
potential for person-to-person transmission, standard precautions must be used
when caring for patients with anthrax.
The 2001 attack
Twenty-two confirmed or
suspected cases of anthrax occurred during the Fall 2001 attack. The patients
are believed to have been infected with anthrax spores distributed through the
U.S. mail. The average incubation period from known exposure to symptoms was
4 days. Eleven patients had inhalational anthrax. Fever, chills, drenching sweats,
profound fatigue, minimally productive cough, nausea and vomiting, and chest
discomfort were symptoms reported by most patients. Six of the 11 patients with
inhalational anthrax survived the 2001 attacks, primarily due to early diagnosis
and intensive supportive care. Another eleven patients had cutaneous anthrax.
Exposure to contaminated mail was the apparent source of infection in all patients
with the cutaneous form of the disease. The incubation period ranged from 1
to 10 days. The initial symptom was often a papule or pimple resembling an insect
bite that developed into a blister-like elevation on the skin. The blisters
then ruptured to form depressed ulcers, often with local edema, ultimately forming
dry black scabs known as eschars. Cutaneous anthrax is painless and does not
produce a rash.
© RnCeus.com
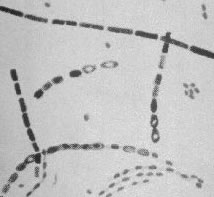 Anthrax is caused by infection with Bacillus anthracis, a gram-positive
spore-forming rod. The spore form of anthrax can survive in the environment
for many decades. Anthrax spores can be distributed in an aerosol form and are
quite resistant to environmental degradation. Anthrax spores from 2 to 6 microns
in size are the ideal size for infecting the mucosal surfaces of the lower respiratory
tract. Manufacturing and distributing anthrax spores in this size range, while
avoiding clumping together of larger spore particles, is one of the challenges
facing bioterrorists attempting to use anthrax as a weapon of mass destruction.
Both bacilli rods and spores are shown in this picture.
Anthrax is caused by infection with Bacillus anthracis, a gram-positive
spore-forming rod. The spore form of anthrax can survive in the environment
for many decades. Anthrax spores can be distributed in an aerosol form and are
quite resistant to environmental degradation. Anthrax spores from 2 to 6 microns
in size are the ideal size for infecting the mucosal surfaces of the lower respiratory
tract. Manufacturing and distributing anthrax spores in this size range, while
avoiding clumping together of larger spore particles, is one of the challenges
facing bioterrorists attempting to use anthrax as a weapon of mass destruction.
Both bacilli rods and spores are shown in this picture. Human anthrax
has three major clinical forms: cutaneous anthrax, inhalation anthrax, and gastrointestinal
anthrax. Cutaneous anthrax occurs when the bacillus is introduced through the
skin; inhalation anthrax, through the respiratory tract; and gastrointestinal
anthrax, by ingestion. Most anthrax cases are cutaneous forms of the disease.
Human anthrax
has three major clinical forms: cutaneous anthrax, inhalation anthrax, and gastrointestinal
anthrax. Cutaneous anthrax occurs when the bacillus is introduced through the
skin; inhalation anthrax, through the respiratory tract; and gastrointestinal
anthrax, by ingestion. Most anthrax cases are cutaneous forms of the disease.
