Neuropathic pain
Neuropathic pain is now defined by the International Association for the Study of Pain (IASP) as ‘pain caused by a lesion or disease of the somatosensory nervous system’ (Murnion, 2018).
Neuropathic pain usually has one or more of the following characteristics:
- pain that persists longer than three months or well beyond healing
- pain without apparent external noxious stimulus
- pain triggered by innocuous stimulus such as light touch (allodynia)
- pain disproportional to stimulation (hyperalgesia)
- pain accompanied by inappropriate
sensations (paresthesia).
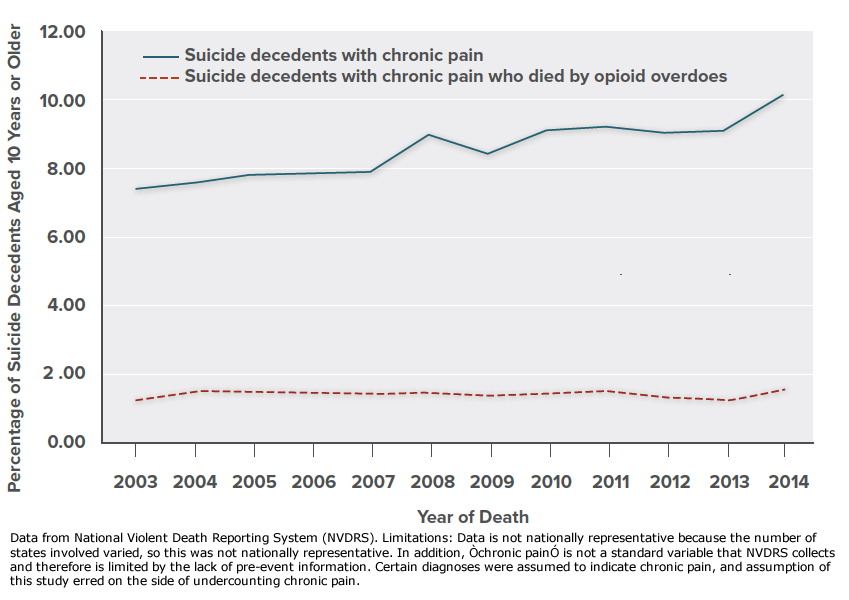 Chronic pain is associated with decreased function, lower quality of life, and other comorbid problems including depression and substance use disorder, and research suggests that pain increases risk for suicide behaviors including death by suicide.
Chronic pain is associated with decreased function, lower quality of life, and other comorbid problems including depression and substance use disorder, and research suggests that pain increases risk for suicide behaviors including death by suicide.
(Click graphic to expand and again to minimize)
Neuropathic pain may be classified by lesion location:
- Central Pain Syndrome (CPS) is a neurological condition caused by physical injury or harm to the central nervous system (CNS), e.g., brain, brainstem, or spinal cord. A CNS injury or lesion can induce to chemical, structural, and functional changes that increase the responsiveness of CNS neurons to afferent (incoming) nociceptor stimulation and also inhibit the CNS modulation of pain by the descending spinal pathways. These changes can present as:
- hyperalgesia reflects increased pain at normal threshold stimulation,
- allodynia reflects pain caused by stimulus that does not usually provoke pain,
- global sensory hyperresponsiveness reflects pain provoked by external stimuli e.g., bright lights, loud noises, smells, foods, and medications (Volcheck, 2023).
A partial list of conditions that have been associated with CPS include:
| Causes Central Pain Syndrome |
- Stroke
- Multiple sclerosis
- Cancer affecting the brain or central nervous system
- Spinal cord injury
- Physical trauma
- Exposure to radiation or certain toxins, such as lead or mercury Infection (bacterial or viral)
|
- Cervical myelopathy
- Neurofibromatosis-1
- Neurofibromatosis-2
- Posterior or transverse myelitis
- Syringomyelia
- Tethered cord syndrome
- Vascular or arteriovenous malformations
- Vitamin B12 deficiency
- Any condition that causes nerve demyelination or other nerve or brain damage
|
| Source: Northwestern Medicine. (n.d.). Central pain syndrome causes and diagnoses. https://www.nm.org/conditions-and-care-areas/neurosciences/central-pain-syndrome/causes-and-diagnoses |
CPS Prevalence
The Cleveland Clinic estimates the occurence rate of CPS for the following conditions:
- Stroke: 8% to 10%.
- Spinal cord injuries: 20% to 40%.
- Multiple sclerosis: ≈30% (Central pain syndrome. n.d.).
CPS symptoms are often experienced as a mix of persistant and painful sensations involving large body areas. Dysesthesias (spontaneous or evoked burning pain, often with a superimposed lancinating component) are typical, but pain may also be deep and aching. Other sensations—eg, hyperesthesia, hyperalgesia, allodynia (pain due to a nonnoxious stimulus), and hyperpathia (particularly unpleasant, exaggerated pain response)—may also occur (Watson, 2023).
CPS Interventions
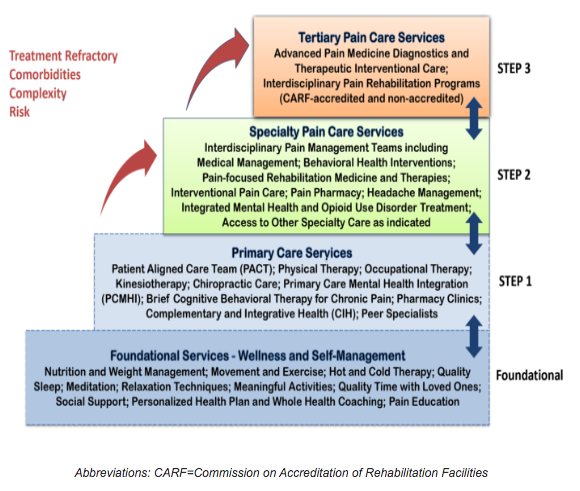 There is currently no cure for CPS, therefore symptom management and improved quality of life are the treatment outcome goals. The Veterans Administration utilizes the multimodal, Stepped Care Model for Pain Management (SCM-PM) to provide whole person pain care. Nurses are intergral to the patient teaching, pain assessment, monitoring and treatment at every step of this model.
There is currently no cure for CPS, therefore symptom management and improved quality of life are the treatment outcome goals. The Veterans Administration utilizes the multimodal, Stepped Care Model for Pain Management (SCM-PM) to provide whole person pain care. Nurses are intergral to the patient teaching, pain assessment, monitoring and treatment at every step of this model.
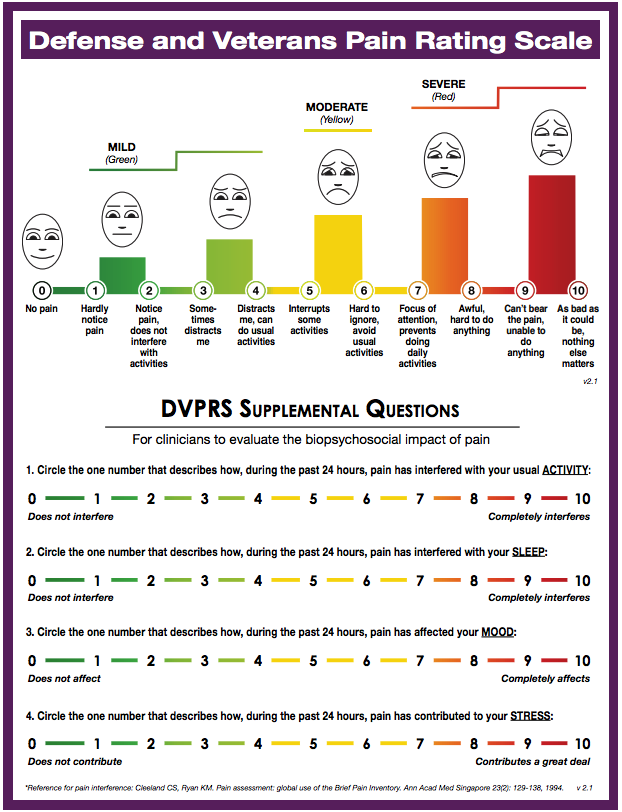 Pain assessment begins with the patient's subjective description of the source, location, & duration of the pain. The following factors can be important to understanding patient pain:
Pain assessment begins with the patient's subjective description of the source, location, & duration of the pain. The following factors can be important to understanding patient pain:
- description of the pain: aching, shooting, gnawing, tender, throbbing, stabbing, sharp, burning, dull
- frequency of the pain: intermittent, constant, periodic, episodic
- intensity of the pain (0-10 subjective rating scale): now, on the average, at its best or worst (i.e., range from minimum to maximum)
- pattern to the pain: in the a.m. vs. p.m., after activity, while distracted, in certain weather
- factors that make the pain worse: overactivity, underactivity, weather, stress, anxiety, muscle tension
- factors that manage the pain: ice, heat, exercise, rest, relaxation, distraction
- medication that has been helpful: NSAIDS, opioids, herbal remedies
- interventional procedures that have been helpful: spinal blocks, surgery, trigger point injections
- behavioral strategies that have been helpful: rest, relaxation, abdominal breathing, meditation, yoga, biofeedback, imagery, hypnosis, exercise, stretching, pacing, pleasant activities, use of positive or realistic self-talk.
Pain Management requires an individualized treatment plan that usually involves both medication and non-drug interventions, along with general guidelines for healthy living, i.e., good nutrition, moderate exercise and stretching, mental stimulation and diversion, social time with friends and family, etc. (Central pain syndrome, n.d.).
Phamacological therapies are individualized to address the specific needs of the patient. The usual pain medication, NSAIDs, and opioids are often inadequate to control CPS symptoms. Multimodal treatment with non-opioid medications commonly used include:
- acetaminophen,
- nonsteroidal anti-inflammatory drugs NSAIDs,
- antidepressants (e.g., serotonin-norepinephrine reuptake inhibitors (SSRI),
- tricyclic antidepressants,
- anticonvulsants,
- musculoskeletal agents,
- biologics,
- topical analgesics
- and anxiolytics
- Ketamine
- Cannabis
The varied mechanisms of action of these medications may be used in combination to produce a synergistic effect (Pain management best practices - hhs.gov. 2019).
Non-pharmacological interventions (see the VA Stepped Care Model for Pain Management (SCM-PM) above)
- Cognitive behavioral therapy (CBT)
- Physical therapies
- Acupuncture
- Deep brain stimulation (DBS)
- Frequency-specific microcurrent (FSM)
- Transcranial magnetic stimulation (TMS)
- Transcutaneous electrical nerve stimulation (TENS), (Central Pain Syndrome. n.d.
Differentiate CPS from CSS |
Condition |
CPS |
CSS |
Definition |
Chronic perception of pain that originates within the CNS |
A normal CNS physiological response to persistent nociception that results in amplification of pain perception. |
Etiology |
Injury or disruption of CNS tissue |
Peripheral injury, inflammation, or chronic pain |
Pain |
Always present |
May or may not be present |
Symptoms |
Widespread pain, hyperalgesia, allodynia |
Hyperalgesia, allodynia, (widespread pain may not be present) |
- Central sensitization Syndrome (CSS) is a normal physiological response of the CNS to persistent nociception, that results in the amplification of the perception of pain. CSS may encompass the sensory input from across many organ systems, causing a myriad symptoms. The effects of CSS can be extensive, generating autonomic, endocrine and immune system disorders that present as: depression, fatigue, sleep disorders, parethesias, cognitive difficulties, bowel and bladder disorders, and other chronic overlapping pain conditions.
- CSS is associated with allodynia, an increased responsiveness of nociceptors to stimuli that would not normally cause pain. This can lead to allodynia, which is the perception of pain from normally non-painful stimuli.
- CSS is associated with neurological changes in the dorsal horn of the spinal cord. The dorsal horn is the part of the spinal cord that receives pain signals from the body. In people with central sensitization, there are changes in the dorsal horn that make it more likely for pain signals to be transmitted to the brain. This can lead to hyperalgesia, which is an increased intensity of pain from normally painful stimuli.
- CSS is associated with changes in the brain that make it more likely for pain signals to be perceived as intense and unpleasant. This can lead to a number of symptoms, including fatigue, sleep disorders, paresthesias, cognitive difficulties, and anxiety.
There is strong evidence that CSS is a major contributor to the development and maintenance of chronic pain. Research is ongoing to determine the exact mechanisms of CSS to develop more effective treatments for chronic pain.
- Peripheral neuropathic pain (PNP) is a common chronic pain condition with major impact on quality of life. It is the result of a lesion or disease involving a sensory nerve or nerves in the somatosensory nervous system encompassing the peripheral nociceptor neurons all the way to their connection to the dorsal horn of the spinal cord.
PNP evolves from somatosensory nerve damage that generates persistant afferent action potentials. The persistant stimulation induces physiologic changes in the peripheral nerve(s) (peripheral sensitization) and physiologic changes in at the synapses within the dorsal horn of the spinal cord (central sensitization). These changes amplify spontaneous or stimulus-dependent afferent activity from damaged or adjacent nerve fibers.
It is theorized that damaged peripheral neurons respond to injury by:
- Reduced primary afferent threshold induced by activation of acid-sensing ion channels (ASIC) in response to substances associated with cellular injury or ischemia. ASICs permit primarily Na+ influx. Upregulation of ASICs increases intracellular Na+ content of the injured nerve, which makes it easier to depolarize (Bennet, M. 2010)
- Remodeling of axon membrane ion channels including Na+, Ca++ and K+ further reduces depolarization threshold (Bennett, M. 2010).
- Demyelination and neuroma formation promote ectopic depolarization and crosstalk from nociceptive to non-nociceptive neurons (Roza, C. 2022)
- Increased primary afferent depolarization increases synaptic neurotransmitters which causing chaotic dorsal horn activity (Bennet, M. 2010).
- A-beta (Aß) fibers (touch) may undergo a phenotype switch, and start expressing substance P (Core Curriculum for Professional Education in Pain, 2005).
PNP treatment
Medications: PAIN MANAGEMENT BEST PRACTICES INTER-AGENCY TASK FORCE REPORT indicates that non-opioid medications can used synergistically to mitigate and minimize opioid exposure. Clinicians must ensure that patients are aware of and discuss all their medications, prescribed and over-the-counter, with their doctor or pharmacist.
- Acetaminophen may be useful for mild to moderate pain but requires awareness of potential liver toxicity.
- NSAIDs effective for acute pain caused by injury or surgery and inflammation, such as from arthritis, bone fractures or tumors, muscle pains, headache.
- Anticonvulsants part of a multimodal plan for postherpetic neuralgia, peripheral neuropathy, and migraine, include: gabapentinoids such as gabapentin and pregabalin.
- Musculoskeletal agents including: baclofen, tizanidine, and cyclobenzaprine .
- Antianxiety medication to treat the anxiety disorders that can accompany acute pain and chronic pain. It is estimated anxiety may impact up to 30% of patients with chronic pain. Benzodiazepines should be avoided due to:
- Risk for abuse
- The risk of overdose, respiratory depression, and death increase when taken with opioids.
- Long-term use can induce cognitive effects that interfere with the pain coping skills
- Antidepressants,
- tricylic antidepressants may be effective an for neuropathic pain
- selective serotonin reuptake inhibitors (SSRI) and Serotonin and norepinephrine reuptake inhibitors.
- Opioid therapy should be initiated when the patient and the clinician deem the benefits outweigh the risks, should be at a low dose and titrated upward to find the lowest dose required to optimally control the pain or improve function and QOL.
Restorative Therapies
- Therapeutic exercise can help patients understand and overcome fear of movement and anxiety that contribute to pain and disability.
- Transcutaneous electric nerve stimulation (TENS), few high quality studies support TENS effectiveness
- Massage therapy may provide effective relief
- Traction for small back pain lacks high quality supportive research.
- Cold and heat application evidence indicates that these modalities may be most effective for acute pain
- Therapeutic ultrasound (TU), there is some evidence that it may be effective for knee osteoarthritis
- Bracing with non-rigid support for short periods may be helpful
Interventional procedures
- Cryoneuroablation is indicated for numerous persistent and intractable painful conditions, including paroxysmal trigeminal neuralgia, chest wall pain.
- Radiofrequency ablation has value in the management of a variety of pain syndromes
- Peripheral nerve injections of local anesthetic agents frequently mixed with anti-inflammatory steroid medication or clonidine for both diagnostic and therapeutic pain relief purposes, and diminishing or preventing the development of chronic pain syndromes.
- Sympathetic nerve blocks (SNBs), injections of local anesthesia at the sympathetic nerve chain has been used to treat neuropathic pain, chronic abdominal, pelvic, and perineal pain.
- Neuromodulation techniques stimulate central or peripheral nervous system tissue for chronic pain treatment, including neuropathic pain, and for both the central and peripheral nervous systems.
- Intrathecal Medication Pumps provide significant analgesia at much lower doses than oral opioids for cancer and non-cancer pain.
- Vertebral augmentation stabilizes the spine through the application of cement to vertebral compression fractures that are painful and refractory to medical treatment.
- Trigger points are palpable, tense bands of skeletal muscle fibers that, upon compression, are capable of producing both local and referred pain.
- Joint Injections of corticosteroid injections into shoulder, elbow, wrist, knee, ankle are common interventional procedures, particularly in the treatment of inflammatory arthritis and basal joint arthritis.
- Interspinous Process Spacer Devices interspinous process spacer devices can provide relief for patients with lumbar spinal stenosis with neuroclaudication.
- Regenerative/adult autologous stem cell therapy offers a potential alternative to long-term opioid therapy.
Instant
Feedback:
Neuropathic
pain stops after healing occurs.
Reference
Bennett, M. (2010). Neuropathic pain. OUP Oxford.
Central neuropathic pain syndromes - mayo clinic proceedings. (2016). https://www.mayoclinicproceedings.org/article/S0025-6196(16)00073-2/fulltext
Central pain syndrome. (n.d.) Cleveland Clinic . https://my.clevelandclinic.org/health/diseases/6012-central-pain-syndrome
Core Curriculum for Professional Education in Pain, edited by J. Edmond Charlton, IASP Press, Seattle, © 2005.
Finnerup, N.B., Kuner, R., Jensen, T.S., (2020) Neuropathic pain: From mechanisms to treatment. https://journals.physiology.org/doi/full/10.1152/physrev.00045.2019
Haverfield, M. C., Giannitrapani, K., Timko, C., & Lorenz, K. (2018). Patient-Centered Pain Management Communication from the Patient Perspective. Journal of general internal medicine, 33(8), 1374–1380. https://doi.org/10.1007/s11606-018-4490-y
Murnion B. P. (2018). Neuropathic pain: current definition and review of drug treatment. Australian prescriber, 41(3), 60–63. https://doi.org/10.18773/austprescr.2018.022
National Institute of Neurological Disorders and Stroke. NINDS Central Pain Syndrome Information Page. accessed 12/2/13 http://www.ninds.nih.gov/disorders/central_pain/central_pain.htm
Neuropathic Pain / Edition 2 by Michael Bennett 2011 Oxford University Press, USA
Northwestern Medicine. (n.d.). Central pain syndrome causes and diagnoses. https://www.nm.org/conditions-and-care-areas/neurosciences/central-pain-syndrome/causes-and-diagnoses
Pain management best practices - hhs.gov. (2019). https://www.hhs.gov/sites/default/files/pmtf-final-report-2019-05-23.pdf
Roza, C.,; Bernal, L. (2022). Electrophysiological characterization of ectopic spontaneous discharge in axotomized and intact fibers upon nerve transection: A role in spontaneous pain? Pflügers Archiv - European Journal of Physiology, 474(4), 387–396. https://doi.org/10.1007/s00424-021-02655-7
Stokes, L. (2018). ANA Position Statement: The Ethical Responsibility to Manage Pain and the Suffering It Causes. American Nurses Association. Retrieved from https://doi.org/10.3912/OJIN.Vol24No01PoSCol01
Ueda, H. (2008) Peripheral mechanisms of neuropathic pain – involvement of lysophosphatidic acid receptor-mediated demyelination. Molecular Pain, 4:11 accessed online 12/1/13 http://www.molecularpain.com/content/4/1/11
Volcheck, M. M., Graham, S. M., Fleming, K. C., Mohabbat, A. B., & Luedtke, C. A. (2023). Central sensitization, chronic pain, and other symptoms: Better understanding, better management. Cleveland Clinic Journal of Medicine. https://www.ccjm.org/content/90/4/245
Watson, J. C. (2023, November 12). Neuropathic pain - neurologic disorders. Merck Manuals Professional Edition. https://www.merckmanuals.com/professional/neurologic-disorders/pain/neuropathic-pain
©RnCeus.com
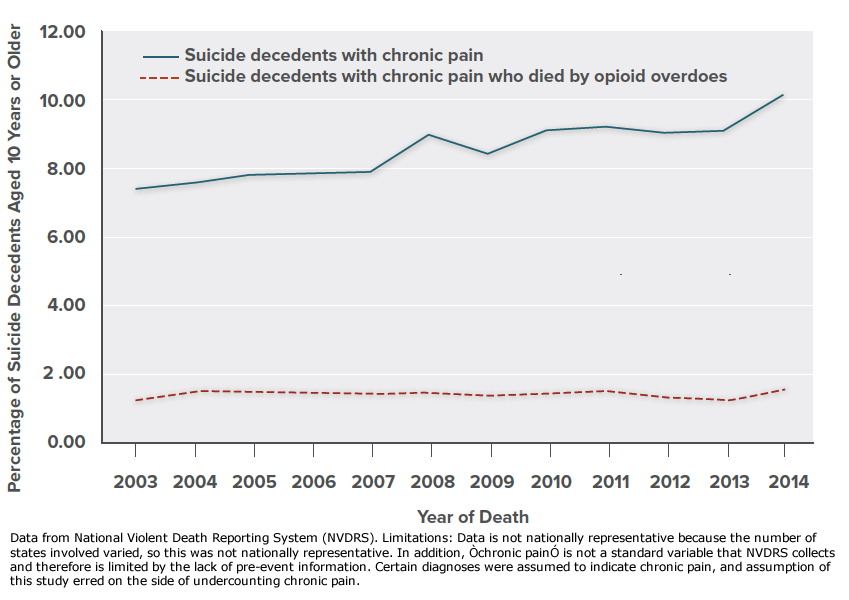 Chronic pain is associated with decreased function, lower quality of life, and other comorbid problems including depression and substance use disorder, and research suggests that pain increases risk for suicide behaviors including death by suicide.
Chronic pain is associated with decreased function, lower quality of life, and other comorbid problems including depression and substance use disorder, and research suggests that pain increases risk for suicide behaviors including death by suicide. 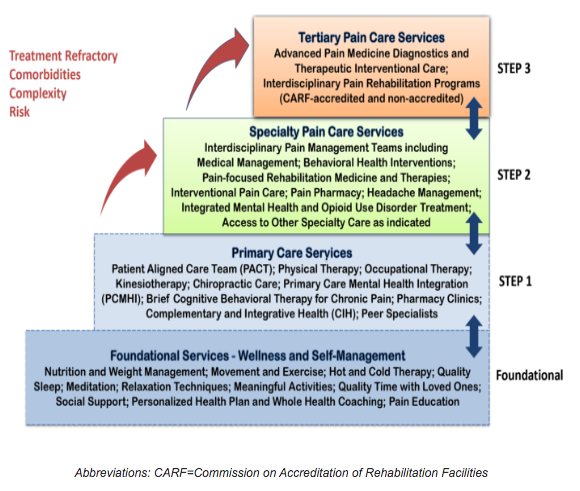 There is currently no cure for CPS, therefore symptom management and improved quality of life are the treatment outcome goals. The Veterans Administration utilizes the multimodal, Stepped Care Model for Pain Management (SCM-PM) to provide whole person pain care. Nurses are intergral to the patient teaching, pain assessment, monitoring and treatment at every step of this model.
There is currently no cure for CPS, therefore symptom management and improved quality of life are the treatment outcome goals. The Veterans Administration utilizes the multimodal, Stepped Care Model for Pain Management (SCM-PM) to provide whole person pain care. Nurses are intergral to the patient teaching, pain assessment, monitoring and treatment at every step of this model.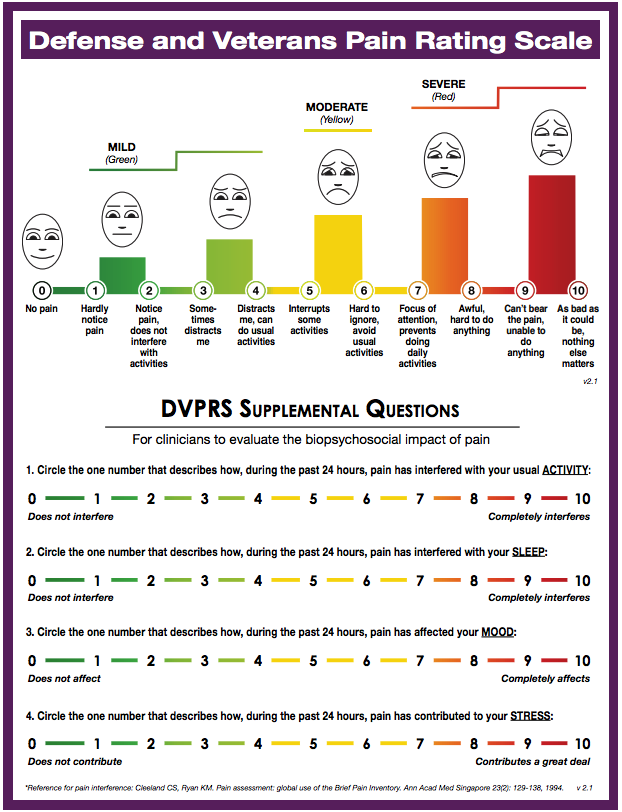 Pain assessment begins with the patient's subjective description of the source, location, & duration of the pain. The following factors can be important to understanding patient pain:
Pain assessment begins with the patient's subjective description of the source, location, & duration of the pain. The following factors can be important to understanding patient pain: