Chaddha et al, (2016) state people who are depressed are twice as likely to those who are not depressed to develop a myocardial infarction. Lichtman et al. (2008) assert that more than 60 prospective studies and numerous meta-analyses have linked depression with reduced prognosis for individuals with coronary heart disease.
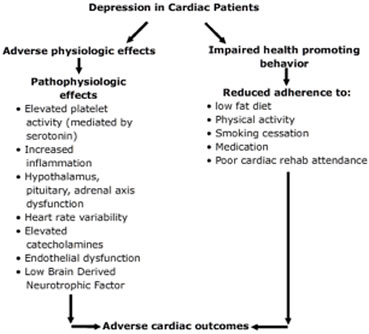 Chronic depression has been associated with the progression of coronary artery disease, decreased health-related quality of life, poor physical functioning, recurrent cardiac events, and a 2 to 2.5 fold increased risk of mortality (Chauvet-Gelinier & Bonin, 2017). Depression often impairs adherence to health behaviors and promotes adverse physiological effects including inflammation, endothelial dysfunction, platelet hyperactivity, and autonomic nervous system abnormalities, all of which can cause adverse cardiac outcomes. Pharmacologic and psychotherapeutic interventions appear to be safe and effective at reducing depressive symptoms in patients with cardiovascular disease and may improve cardiac outcomes (Teply, et al., 2016).
Chronic depression has been associated with the progression of coronary artery disease, decreased health-related quality of life, poor physical functioning, recurrent cardiac events, and a 2 to 2.5 fold increased risk of mortality (Chauvet-Gelinier & Bonin, 2017). Depression often impairs adherence to health behaviors and promotes adverse physiological effects including inflammation, endothelial dysfunction, platelet hyperactivity, and autonomic nervous system abnormalities, all of which can cause adverse cardiac outcomes. Pharmacologic and psychotherapeutic interventions appear to be safe and effective at reducing depressive symptoms in patients with cardiovascular disease and may improve cardiac outcomes (Teply, et al., 2016).
Huffman, Celano, Beach, Motiwala, Januzzi (2013) developed a model describing the potential mechanisms linking depression and cardiac disease (above). They concluded depression in cardiac patients resulted in the following physiological changes: elevated platelet activity, increased inflammation, hypothalamic–pituitary–adrenal axis dysfunction, decreased heart rate variability, endothelial dysfunction, and Brain-derived neurotrophic factor (BDNF). Depression also impaired health promoting behaviors such as adherence to low-fat diet, exercise, smoking cessation, and medication adherence (Chauvet-Gelinier & Bonin, 2017).
Treatment of depression includes antidepressant drugs, cognitive behavioral therapy, and physical activity.
Antidepressant drugs:
Selective serotonin reuptake inhibitor (SSRI) antidepressants
sertraline (Zoloft), citalopram (Celexa), escitalopram (Lexapro), fluoxetine (Prozac), fluvoxamine (Luvox), and paroxetine (Paxil) are recommended for patients with depression and CAD. Tricyclic antidepressants (TCAs) and monoamine oxidase inhibitors (MAOIs) are not recommended because of their cardiotoxic side effects (Teply, et al., 2016); Glassman et al., 1993).
Comparisons of SSRI antidepressants with TCAs and MOAIs and their cardiovascular side effects continue to be studied. Large studies such as the one by Spindelegger et al. (2014) of 169,278 psychiatric inpatients showed MOA inhibitors to have the most cardiotoxic effects, followed by tricyclic antidepressants with the least cardiotoxic effects of the SSRI antidepressants.
Teply, et al. (2016) reviewed several studies of antidepressant medications. They found the new selective serotonin reuptake inhibitors (SSRIs) to be well tolerated, with good efficacy in cardiovascular patients.
Taylor et al. (2005) examined the effects of antidepressant medication on the morbidity and mortality of 1,834 post MI patients. Mortality or recurrences of MI was significantly lower in patients taking SSRIs than non-users of antidepressants or those taking non SSRI medications. Similar results were found by Mavrides & Nemeroff (2013) in their review of 61 articles about the use of antidepressants with patients with CAD.
Zhang, Chen, Ma (2018) found geriatric depression as a prevalent risk factor associated with morbidity and mortality of cardiovascular disease. Antidepressive therapy, improvement in psychological and social function continue to be investigated for efficacy in reducing increased cardiovascular risk in the elderly population.
 Additional researchers found patients in the American Heart Association Heart Failure (HF) stages C and D have additional challenges with depression. Patients with heart failure and those undergoing implantable cardioverter-defibrillator (ICD) placement have an increased risk of depression. They exhibit a combined score of 56% for depressive symptoms and MDD (Rutledge et al., 2006; Magyar-Russell et al. 2011). In addition, patient’s undergoing coronary artery bypass graft surgery (CABG) show increased symptoms of depression (Tully & Baker, 2012). The depression has been shown to impact negatively on adjustments to devices and recovery from surgery.
Additional researchers found patients in the American Heart Association Heart Failure (HF) stages C and D have additional challenges with depression. Patients with heart failure and those undergoing implantable cardioverter-defibrillator (ICD) placement have an increased risk of depression. They exhibit a combined score of 56% for depressive symptoms and MDD (Rutledge et al., 2006; Magyar-Russell et al. 2011). In addition, patient’s undergoing coronary artery bypass graft surgery (CABG) show increased symptoms of depression (Tully & Baker, 2012). The depression has been shown to impact negatively on adjustments to devices and recovery from surgery.
Foss-Nieradko, Stepnowska, & Piotrowicz (2012) conducted a prospective comparison on the effects of chronic depression, incidental depression, and no depression on outcomes after coronary artery bypass grafting. After a two-year study, they found cardiac events occurred more frequently among patients with chronic depression but not incidental depression when compared with patients with no depressive symptoms.