Treatment
Historically, DCIS was understood to be a precursor to invasive ductal carcinoma and was treated aggressively with mastectomy. Beginning in the 1970's evidence supporting the efficacy of breast sparing wide local excision (lumpectomy) shifted treatment away from mastectomy.
Today we know that the progression from low grade (low risk) to higher grade (higher risk) lesions is not linear. Some lesions never progress to invasive ductal carcinoma. The DCIS treatment paradigm is likely to shift again based upon new data published by Narod, et al (2015). Their findings indicate significant other factures besides the presence of DCIS influence survival rate. These factors include the following:
- The twenty-year overall risk of death from breast cancer following a diagnosis of DCIS was 3.3%.
- The breast cancer mortality rate post-DCIS diagnosis was more than twice as high for women diagnosed before age 35.
- The breast cancer mortality rate post-DCIS diagnosis for black women was more than double that of white women.
- The breast cancer mortality rate post-DCIS diagnosis following a subsequent diagnosis of primarly primarily ipsilateral invasive breast cancer was about 18%.
- DCIS treatment with both lumpectomy and radiation reduced the post-DCIS diagnosis recurrence rate to 2.5% versus 4.9% for lumpectomy alone but it did not affect the breast cancer mortality rate.
- A small number of post-DCIS diagnosis deaths were attributed to breast cancer metastasis with no evidence of invasive breast cancer in the breasts.
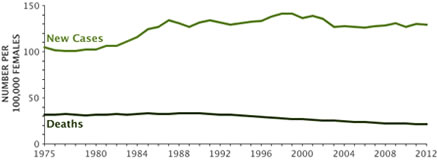 This data by Narod, et al. have rekindled the controversy over the optimum treatment of DCIS. Proponents of aggressive therapy credit surgical excision of DCIS lesions for the trend of decreasing breast cancer mortality, depicted in the chart to the right. Proponents of less aggressive therapy believe that technology has compelled the identification and excision of smaller and smaller DCIS lesions which present little or no risk of mortality. They counsel patients to wait and see if their small low-grade lesions will progress to higher grade lesions with greater risk before initiating treatment. The new paradigm reserves initial aggressive therapy for DCIS lesions in women younger than 35-40 years, black women and women with genetic mutations that predispose to invasive breast cancer.
This data by Narod, et al. have rekindled the controversy over the optimum treatment of DCIS. Proponents of aggressive therapy credit surgical excision of DCIS lesions for the trend of decreasing breast cancer mortality, depicted in the chart to the right. Proponents of less aggressive therapy believe that technology has compelled the identification and excision of smaller and smaller DCIS lesions which present little or no risk of mortality. They counsel patients to wait and see if their small low-grade lesions will progress to higher grade lesions with greater risk before initiating treatment. The new paradigm reserves initial aggressive therapy for DCIS lesions in women younger than 35-40 years, black women and women with genetic mutations that predispose to invasive breast cancer.
Current therapeutic approaches for DCIS
According to Doke, Butler & Mitchell (2018) the following options are recommended for patients with DCIS:
- Surgical management options include breast conservation, mastectomy, or possibly nipple sparing mastectomy.
- Radiation therapy is recommended as a component of breast conserving therapy for patients with DCIS
- In low risk patients trial data suggests adjuvant radiation may be omitted
- Endocrine therapy is offered to women with hormone positive DCIS who have undergone lumpectomy
- Studies have explored use of targeted treatments such as trastuzumab in DCIS for HER2 overexpression.
New information about importance of wide margins from surgery
Van Zee, et al (2015) studied 2996 cases of women with DCIS. 363 patients had recurrences. The recurrences were considerably less in women who had wide negative margins from surgery. Women with wide negative margins and radiation therapy had the lowest recurrence rates. The researchers concluding wider negative margins to be important in reducing risk for women choosing not to have RT. Wider margins may not be necessary for those receiving RT.
DCIS Management Options
- Active surveillance without endocrine therapy following core needle biopsy and pathological grading and staging. (This is not the standard of care but may be offered to some women on an individual basis.)
- Active surveillance coupled with endocrine therapy for estrogen receptor (+) DCIS is not an accepted management option but might offer benefit to a small number of patients who refuse surgical intervention. Endocrine therapy consisting of SERMs like tamoxifen or raloxifene for premenopausal women or an aromatase inhibitor for postmenopausal women are being investigated but the long term effect on disease free survival remains unknown (Meyerson, et al. 2011).
- Lumpectomy followed by radiation seems to be equally as effective as mastectomy for people with only one site of cancer in the breast and a tumor under 4 centimeters. Clear margins are also a requirement (Frank, et al., 2016).
- DCIS by definition is non-metastatic, as such, there is no role for cytotoxic chemotherapy in the treatment of DCIS. (Kim, et al., 2018).
 DCIS management is determined by: lesion size, focal vs multifocal, histological grade, estrogen receptor status, presence of microinvasion, patient age and preference. Historically, DCIS was treated with simple mastectomy. The goal of mastectomy is to reduce the risk of invasive carcinoma and post-surgical recurrence by the removing the majority of breast tissue including the entire DCIS lesion. The local-regional control rates of DCIS by mastectomy are reported as 96%-100%. (Narad, et al., 2015).
DCIS management is determined by: lesion size, focal vs multifocal, histological grade, estrogen receptor status, presence of microinvasion, patient age and preference. Historically, DCIS was treated with simple mastectomy. The goal of mastectomy is to reduce the risk of invasive carcinoma and post-surgical recurrence by the removing the majority of breast tissue including the entire DCIS lesion. The local-regional control rates of DCIS by mastectomy are reported as 96%-100%. (Narad, et al., 2015).
Immediate post mastectomy reconstructive surgery is an option for many women. Modern skin sparing and nipple preserving mastectomy options can offer improved aesthetic outcomes. Nipple preserving procedures may even preserve sensation. Insurers who cover mastectomy are required by federal law to also cover breast reconstruction. That includes procedures needed to achieve a balanced appearance between the two breasts. For more information about breast reconstruction check out this website, https://www.breastcancer.org/treatment/surgery/reconstruction/is-reconstruction-for-you
While the simple mastectomy cure rate for DCIS is high, it may be more aggressive therapy than some women want or require. Today, breast conserving surgery (lumpectomy) combined with post-operative whole breast radiation therapy offers long term survival statistics similar to mastectomy. The addition of adjuvant endocrine therapy has been demonstrated to reduce the risk of local recurrence and the development of new contralateral and ipsilateral breast cancers but does not increase the long term survival rate. (Barrio, 2017).
In general, larger breasts may achieve a better cosmetic effect from breast conserving techniques. The percentage of breast volume excised may be an important determinant of cosmesis and patient satisfaction after breast-conserving surgery.• (Cochrane, 2003). Smaller breasts may achieve a better cosmetic effect from mastectomy with reconstruction.
Selecting mastectomy over breast conserving surgery: (Barrio, 2017)
- Recurrence or new DCIS lesions after breast conserving surgery
- Diffuse mammographic calcifications suggesting extensive disease
- Multicentric lesions
- Inability to obtain clear margins with breast conserving surgery
- Likelihood of poor cosmetic outcome after breast conserving surgery
- Patient preference
- Contraindications to adjunctive breast radiation therapy
- Previous irradiation of chest wall
- Collagen vascular disease (scleroderma or lupus)
- Severe heart or lung disease
- First or second trimester pregnancy
- Axillary considerations:
- Axillary dissection is usually avoided for DCIS
- Where there is high volume and high-grade DCIS or suspicion of invasive disease sentinel lymph node biopsy to stage the axilla may be considered
 Breast Conserving Surgery (BCS): DCIS Recommendations: (Doke, 2018)
Breast Conserving Surgery (BCS): DCIS Recommendations: (Doke, 2018)
- A circumferential or radial margin of greater than or equal to 2 mm should be achieved where possible
- DCIS extending up to a margin of excision requires additional surgery to achieve clear margins in the absence of contraindications
- Factors influencing the decision to re-excise margins which are less the 2mm include:
- Age
- Size, grade, and the presence or absence of comedo necrosis
- Extent of DCIS approaching the margin
- Radiation oncology should be consulted regarding the need for full breast irradiation following BCS
- Benefits and risks of endocrine therapy should be offered to women with hormone receptor positive ductal carcinoma in situ.
The surgeon
There is considerable research supporting better patient outcomes using surgeons and hospitals that have high volume in the specific surgical area (Birkmeyer, et al, 2002). There are surgeons whose practice specialty is breast surgery. It may be important also for patients to consult a board-certified plastic surgeon who specializes in breast surgery and reconstruction. Currently there is a website called Surgeon Scorecard,
https://projects.propublica.org/surgeons/, which gives surgeon complication rates for 8 procedures. Presently is does not include breast surgery for invasive or in situ cancer. It is just the beginning of this type of disclosure. Check for future increased number of procedures.
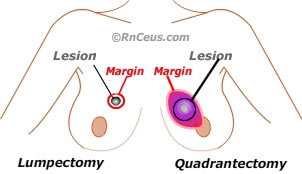
Lumpectomy
Lumpectomy is a procedure (BCS) that intends to surgically remove all disease, suspicious calcifications and at least 2mm of surrounding healthy tissue. If clear margins are not obtained on the initial lumpectomy, re-excision of any positive margins is required. Re-excision rates vary widely depending on multiple factors including the lesion size and the means used to identify lesion perimeters.
Lumpectomy in conjunction with radiation therapy has been shown to reduce local recurrence of DCIS when the mass is about 4 cm in diameter or less. Lumpectomy is often performed in the outpatient setting using local anesthesia. If the breast is large, and position of the mass requires extensive manipulation or sentinel node biopsy is anticipated, general anesthesia may be required.
Mastectomy
Several studies have shown that only 1-2% of women with DCIS will die of breast cancer regardless of whether they were treated with lumpectomy or mastectomy. Therefore, mastectomy is usually reserved for cases where repeated lumpectomies fail to produce clear margins, where there are diffuse malignant appearing microcalcifications or when the breast is small, and resection would result on significant deformity.
Radiation therapy
Radiation therapy involves the delivery of high energy rays to the treatment site. These rays disrupt vascular endothelium in the treatment field resulting in decreased tissue vascularity. The reduced vascularity deprives microinvasive lesions and invasive breast cancer the environment needed for efficient cellular reproduction. (Rudloff, 2009).
Endocrine therapy may be recommended to prevent the recurrence of estrogen (+) lesions.
- Selective Estrogen Receptor Modulators (SERMs) including tamoxifen and raloxifene act like estrogens in some tissues, but block estrogen action in others. Estrogens act through estrogen receptors (ERs) to mediate nuclear transcription. In females, estrogens play a key role in reproduction and induce beneficial effects on the skeletal, cardiovascular, and central nervous systems.• (Guerrieri-Gonzaga, 2016).
The SERMs tamoxifen and raloxifene both exhibit estrogen receptor (ER) antagonist activity in breast and agonist activity in bone, but only tamoxifen manifests agonist activity in the uterus. Common anti-estrogen side effects include: fatigue, hot flashes, night sweats, vaginal discharge, and mood swings.
- Tamoxifen has been shown in a randomized controlled study to reduce the recurrence of invasive breast cancer but it increases the risk of:
- endometrial cancers
- venous thromboembolism
- fatty liver and cirrhosis with long term use
- Raloxifene does not increase the risk of endometrial cancers but has toxic effects similar to tamoxifen
- The mortality rate of women receiving or not receiving SERMS post breast cancer diagnosis is the same (Cuzick, Powles, Veronesi, 2003).
LCIS treatment
Currently lobular carcinoma in situ (LCIS) is not considered to be a precursor to cancer, with research still being carried out to verify or refute that. Treatment of LCIS tends to be surgical incision or lumpectomy with no radiation. What is known is LCIS does signal an increased risk of developing breast cancer higher than the normal female population.
Women with LCIS, especially those with other risk factors, are encouraged to lower whatever risk factors can be reduced and be more diligent about doing self-breast exams and having annual mammograms (Chen, 2017).
Instant feedback:
Women with DCIS who had wide negative margins and radiation therapy had the lowest recurrence rates.
Reference
Barrio, A. V. & Van Zee, K. J. (2017). Controversies in the Treatment of DCIS. Annu Rev Med. 68, 197–211.
Birkmeyer, J.D., Siewers, A.E., Finlayson, E. A., Stukel, T.A., Lucas, F.E., Batista, I., et al. (2002). Hospital volume and surgical mortality in the United States. N Engl J. 346, 1128–1137.
Cheng, P., Huang, P., Shou, J., Hu, G., Han, M. & Huang, J. (2017). Treatment and survival outcomes of lobular carcinoma in situ of the breast: a SEER population-based study. Oncotarget. 8(61), 103047–103054.
Cochrane, R.A., Valasiadou, P., et al. (2003). Cosmesis and satisfaction after breast-conserving surgery correlates with the percentage of breast volume excised. British Journal of Surgery. 90(12),1505-9.
Cuzick, J., Sestak, I., Pinder, S. E., Ellis, I. O., Forsyth, S., Bundred, N.J., et al. (2011). Effect of tamoxifen and radiotherapy in women with locally excised ductal carcinoma in situ: long-term results from the UK/ANZ DCIS trial. Lancet, 12, 21-29.
Doke, K., Butler, S. & Mitchell, M.P. (2018). Current Therapeutic Approaches to DCIS. J Mammary Gland Biol Neoplasia. 23(4), 279-291.
Frank, S., Dupont, A., Teixeira, L., Porcher, R., De Roquancourt, A., Giacchetti, S., et al. (2016). Ductal carcinoma in situ (DCIS) treated by mastectomy, or local excision with or without radiotherapy: A monocentric, retrospective study of 608 women. Breast. 25, 51-6.
Guerrieri-Gonzaga, A., Sestak, I., Lazzeroni, M., Serrano, D., Rotmensz, N., Cazzaniga, M., et al. (2016). Benefit of low-dose tamoxifen in a large observational cohort of high-risk ER positive breast DCIS. Int J Cancer. 139(9), 2127-34.
Kim, C., Liang, L., Wright, F.C., Hook, N. J., Groot, G., Helyer, L. et al. (2018). Interventions are needed to support patient–provider decision-making for DCIS: a scoping review. Breast Cancer Res Treat. 168(3), 579–592.
Meyerson, A. F., Lessing. J. N., Itakura, K., Hylton, N. M., Joe, B. N. et al. (2011). Outcome of long-term active surveillance for estrogen receptor-positive ductal carcinoma in situ. Science Direct. 20(6), 529-533.
Narod, S., Iqbal, J., et al. (2015). Breast Cancer Mortality After a Diagnosis of Ductal Carcinoma In Situ. Oncology. 1(7), 888-896.
Rudloff, U., Brogi, E., McCormick, B., et al. (2009). The influence of margin width and volume of disease near margin on benefit of radiation therapy after breast-conserving surgery for DCIS: Results of long-term follow-up. Journal of Clinical Oncology. 27(15), 531.
Van Zee, K.J., Subhedar, P., Olcese, C., Patil, S. & Morrow, M. (2015). Relationship Between Margin Width and Recurrence of Ductal Carcinoma In Situ: Analysis of 2996 Women Treated With Breast-conserving Surgery for 30 Years. Ann Surg. 262(4),623-31.
© RnCeus.com
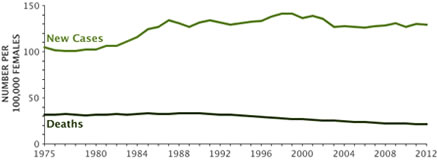 This data by Narod, et al. have rekindled the controversy over the optimum treatment of DCIS. Proponents of aggressive therapy credit surgical excision of DCIS lesions for the trend of decreasing breast cancer mortality, depicted in the chart to the right. Proponents of less aggressive therapy believe that technology has compelled the identification and excision of smaller and smaller DCIS lesions which present little or no risk of mortality. They counsel patients to wait and see if their small low-grade lesions will progress to higher grade lesions with greater risk before initiating treatment. The new paradigm reserves initial aggressive therapy for DCIS lesions in women younger than 35-40 years, black women and women with genetic mutations that predispose to invasive breast cancer.
This data by Narod, et al. have rekindled the controversy over the optimum treatment of DCIS. Proponents of aggressive therapy credit surgical excision of DCIS lesions for the trend of decreasing breast cancer mortality, depicted in the chart to the right. Proponents of less aggressive therapy believe that technology has compelled the identification and excision of smaller and smaller DCIS lesions which present little or no risk of mortality. They counsel patients to wait and see if their small low-grade lesions will progress to higher grade lesions with greater risk before initiating treatment. The new paradigm reserves initial aggressive therapy for DCIS lesions in women younger than 35-40 years, black women and women with genetic mutations that predispose to invasive breast cancer. DCIS management is determined by: lesion size, focal vs multifocal, histological grade, estrogen receptor status, presence of microinvasion, patient age and preference. Historically, DCIS was treated with simple mastectomy. The goal of mastectomy is to reduce the risk of invasive carcinoma and post-surgical recurrence by the removing the majority of breast tissue including the entire DCIS lesion. The local-regional control rates of DCIS by mastectomy are reported as 96%-100%. (Narad, et al., 2015).
DCIS management is determined by: lesion size, focal vs multifocal, histological grade, estrogen receptor status, presence of microinvasion, patient age and preference. Historically, DCIS was treated with simple mastectomy. The goal of mastectomy is to reduce the risk of invasive carcinoma and post-surgical recurrence by the removing the majority of breast tissue including the entire DCIS lesion. The local-regional control rates of DCIS by mastectomy are reported as 96%-100%. (Narad, et al., 2015).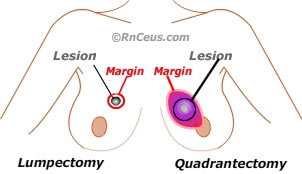 Breast Conserving Surgery (BCS): DCIS Recommendations: (Doke, 2018)
Breast Conserving Surgery (BCS): DCIS Recommendations: (Doke, 2018)